2017 FSA Posters
P018: INNOVATION IN ATRIAL FIBRILLATION ABLATION: THE "CONVERGENT PROCEDURE"
Shashank S Shettar, MBBS, MD, Sanjeev Chhangani, MD, FCCM, MBA; University of Florida, COM Jacksonville
Introduction: Atrial fibrillation (AF) is the most common cardiac arrhythmia. Catheter ablation is indicated in patients with recurrent AF despite optimal medical therapy. With declining success rates, repeated ablations are often required, exposing extended periods of radiation and peri-procedural complications. Traditional open “Maze” procedure requires sternotomy and cardio-pulmonary bypass (CPB). A hybrid procedure, “The Convergent Procedure”, combines catheter-based endocardial and minimally-invasive epicardial ablation into one single operation designed to more effectively treat atrial fibrillation. In this report, we discuss anesthetic considerations and technical complexities of the “Convergent-Procedure”.
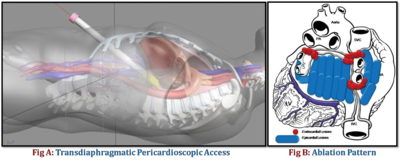
Case Presentation: A 51 year old male with past medical history of morbid obesity (BMI 37), hyothyroidism, diverticulitis, s/p exploratory laparotomy and colostomy, chronic AF s/p ablation presented with persistent symptomatic AF despite maximal medical therapy and three attempts at cardioversion. Preoperative medications included Apixaban and FLecainide. Following evaluation by a multi-disciplinary team of cardiologist, cardio-thoracic surgeon and anesthesiologist, perfusionist, and nursing staff, he was scheduled for the “Convergent-procedure”. After insertion of a radial arterial catheter and two large bore peripheral IV cannula, general endotracheal anesthesia was induced with propofol, fentanyl, and rocuronium. The cardiopulmonary bypass was on standby. A post-induction TEE was done to rule out cardiac thrombus. The TEE probe was then replaced by an esophageal temperature (Eso-T) probe with its tip positioned 2 vertebral bodies below the bifurcation of the carina under fluoroscopic guidance. The pericardium was approached by a sub-xiphoid incision and using CO2 insufflation an endoscopic cannula was placed through diaphragm to access the posterior surface of the heart (figure A). Ablation electrode assembly, introduced via the endoscopic cannula, was used to ablate posterior wall of LA and pulmonary veins. The rhythm converted to sinus by the end of the procedure. A drain was placed into the pericardial space and the incision was closed. The cardiology team then performed endocardial ablation using trans-septal puncture, 3D electro-anatomical mapping and pulmonary vein isolation (figure B). The patient was hemodynamically stable, in sinus rhythm and was extubated at the end of the procedure. He was discharged home in sinus rhythm without any complications.
Discussion: The “Convergent procedure” represents innovation in the therapy of AF, combining minimally-invasive surgical and endocardial catheter ablation. Carefully integrated and collaborative team approach and communication, and well-defined roles are central to the success of this endoscopic complex technique. During endoscopic stage, goals are to maintain a motionless field, prevent hypotension during insufflation and ablation using fluid bolus +/-vasopressor, and being prepared to convert to open cardiac procedure in the event of cardiac injury. The Esophageal temperature monitoring allows safe ablation of atrial structures in close proximity to the esophagus by providing early warning about excessive heating of ablating electrode. During endocardial stage, goals are to monitor the pericardial drain output, monitor anticoagulation, prevent hypotension, and watch for arrhythmias.
References:
Zembala MO, et al. Minimally invasive surgery for atrial fibrillation. Thorac Dis 2013;5:S704-S712
Boersma LV, et al. Atrial fibrillation catheter ablation versus surgical ablation treatment (FAST): a 2-center randomized clinical trial. Circulation 2012;125:23-30
