2017 FSA Posters
P038: SIMULATION-BASED LEARNING IMPROVES ANESTHESIOLOGY RESIDENT CONFIDENCE IN CRITICAL SKILLS: A FLIPPED CLASSROOM APPROACH
Kevin R Olsen, MD, Lucas Bannister, MD, Aneel Deshmukh, MD, Terrie Vasilopoulos, PhD, David J Hall, MD, Juan C Mira, MD, Rohit Patel, MD; UF
INTRODUCTION: Physicians freshly minted emerge from medical with varying confidence and knowledge of practical skills pertaining to the diagnosis and management of common inpatient issues. Examples include the work-up and treatment of altered mental status, advanced cardiac life support(ACLS), and methods of supplemental oxygen delivery. New interns are also often the first physicians to respond to both common complaints and emergencies on floor patients. With varying levels of medical knowledge and practical skills, patients may receive sub-standard care depending on the intern who is caring for them
METHODS: Following IRB approval, a single institution’s resident physicians entering their internship year were assigned instructional videos to watch on the topics of ACLS, supplemental oxygen delivery, bedside trans-thoracic echocardiography, and invasive line placement. They then participated in a 3-day hands-on simulation curriculum throughout which they physically performed the skills described in the videos. We surveyed residents on their confidence in performing across three areas: Procedures, Autonomy, and Medical Knowledge. We compared their post-simulation confidence in both procedural ability and knowledge base to their pre-simulation confidence levels as well as to residents (PGY-2) at the same institution who had just completed their internship and had not undergone any formal instruction or simulation.
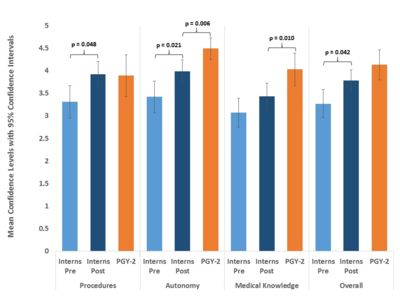
RESULTS: Overall confidence levels (summary of all survey areas) of interns increased from the pre-survey to the post-survey (p=0.042), as well as specifically for Procedures (p=0.048) and Autonomy (p=0.021). After the 3-day simulation curriculum, there were no significant differences in confidence between interns (following simulation) and PGY-2 residents on overall confidence (p=0.069) and in Procedures (p=0.876). However, interns’ confidence was still lower than that of the PGY-2s in Autonomy (p=0.006) and Medical Knowledge (p=0.010).
CONCLUSIONS: Prior to this simulation based curriculum, new interns received cursory training in ACLS, line placement, and supplemental oxygen delivery techniques – skills that are essential to house-staff who are often the first-call for both routine and emergency situations. These knowledge deficits created wide variability in the skill-set of anesthesiology interns resulting in variations in patient care and safety concerns. A simulation-based curriculum utilizing a flipped-classroom model during intern orientation can contribute to a standardized and effective skill-set delivered in a short period, yielding an comparable confidence in implementation of that skill-set, particularly in procedural ability, as one-year of residency.
Figure 1. Mean confidence levels pre- and post-simulation for PGY-1 residents and for PGY-2 residents who had not undergone simulation, for overall confidence and for each area. Error bars indicate 95% confidence intervals. P-values are reported for statistically significant differences (p < 0.05).