2019 FSA Posters
P049: BEST LOCATION AND READER ROLE OF USAGE OF EMERGENCY MANUALS DURING CRITICAL EVENTS: EXPERIENCED EMERGENCY MANUAL USERSâ OPINION
Kyle J Sanchez1, Jeffrey Huang1, Jiayan Wu2, Andrey Suprun1; 1University of Central Florida College of Medicine, 2Zhongstan Traditional Chinese Medicine Hospital
Introduction: Emergency Manuals (EM) are an essential component of the response to critical events by health care providers, and there is abundant evidence to support the benefits of utilizing EMs in crisis management. Despite the growing acceptance of EM incorporation into operating room culture, there is currently no standardized protocol for EM usage. There is also a lack of research focused on maximizing its efficacy, with minimal data on the best methods to incorporate crisis checklists and emergency manuals into everyday practice. To develop a protocol for EM utilization, factors such as the best location for EMs to be placed and the EM reader role must be determined. To our knowledge, no study has been performed to assess the best location for EMs or the preferred reader for EMs during critical events.
Methods: Anesthesiologists with experience in EM use from seven hospitals participated in a survey questionnaire that was distributed to all participants through WeChat using the WenJianxen software. Survey response numbers were converted into percentages and were used to summarize categorical variables.
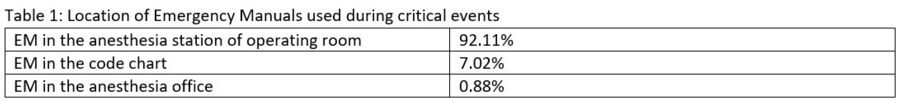
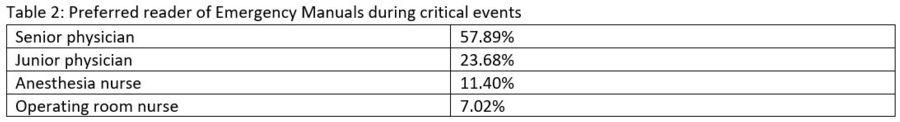
Results: Our survey showed the best location of EMs used during critical events was in the Anesthesia Station of the operating room (Table 1) and that the preferred reader of EMs during critical events is the senior physician (Table 2).
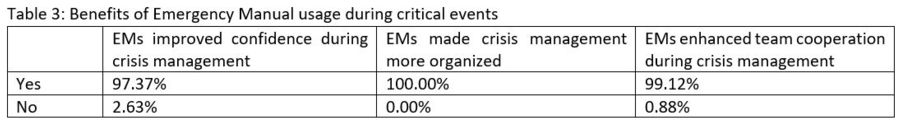
The opinion of respondents on how EMs benefit crisis management is shown in Table 3. Most respondents felt that EMs improved their confidence during crisis management, enhanced team cooperation during crisis management, and made crisis management more organized.
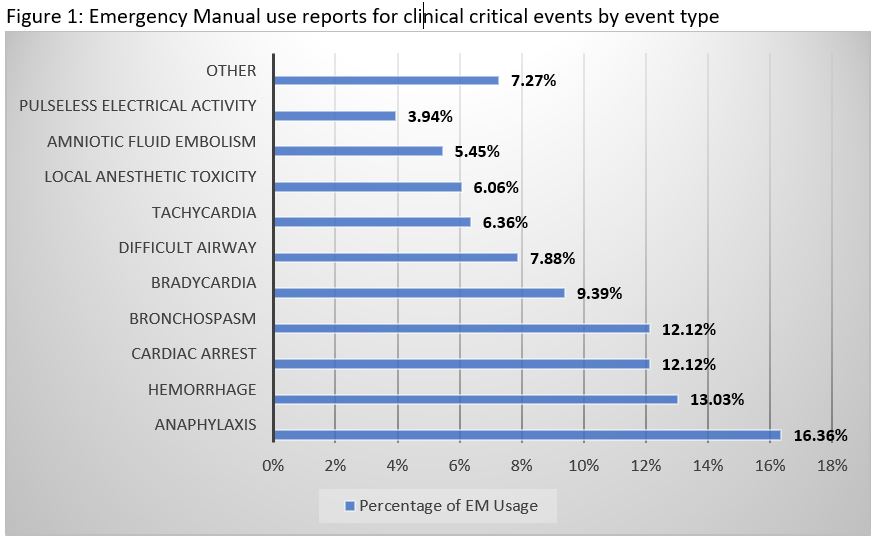
The type of critical events for which EM was most commonly used is shown in Figure 1. Overall, respondents have used the EM most often for anaphylaxis (16.36%), followed by hemorrhage (13.03%), cardiac arrest (12.12%), and bronchospasm (12.12%).
Discussion/Conclusion: We believe that the best location of EMs is one which maximizes efficiency by minimizing the time spent retrieving it. As shown by our results, perhaps the greatest way to minimize the retrieval time is to have the EM located in the operating room itself rather than in the code chart or anesthesia office. Additionally, our study showed that the preferred reader of EMs during critical events is the senior physician, which suggests that the reader should be an experienced team member with a high degree of leadership over the clinical team. Our results may be applicable to the development of a standardized protocol for EM usage which, as suggested by our survey, maximizes efficiency by having the EMs located in the operating room and assigning the reader role to the senior physicians if available.