2019 FSA Posters
P064: PACU MONITORING OF END-TIDAL CO2 (ETCO2 ) IN BARIATRIC PATIENTS AFTER ROUX-EN-Y SURGERY WITH OPIOID SPARING TECHNIQUES
Enrico M Camporesi, MD1, Jin Deng, MS2, Hesham Abowali, MD1, Maha Balouch, BA1, Garrett Enten, BS1, Devanand Mangar, MD3; 1TEAMHealth Anesthesia Research Institute, 2University of South Florida Morsani College of Medicine, 3TEAMHealth Anesthesia
Introduction: About 8% of bariatric surgery patients develop perioperative respiratory complications [1]. Pulse oximetry, which measures peripheral oxygen saturation (SPO2) levels, is commonly utilized during recovery in PACU for respiratory monitoring. But the ability of pulse oximetry to detect hypoventilation is reduced when patients are provided supplemental oxygen to breathe, which can increase SPO2 and mask hypoxemia until critical hypoventilation occurs [2]. Continuous capnography via specialized nasal prongs monitors the partial pressure of CO2 of an expired breath and can be used as a valid alert monitor of respiration. We analyzed capnography in the PACU for an obese population post bariatric surgery.
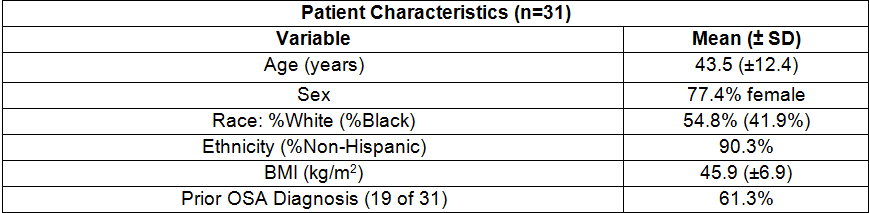
Methods: IRB-approved consent was obtained from 31 Roux-en-Y gastric bypass surgery patients with an average body mass index of 45.9 kg/m2 and a STOP-BANG score from 5-8 (Table 1). Anesthesia was induced with lidocaine and propofol. Patients were intubated with rocuronium. Sevoflurane (1/2 MAC) along with a continuous infusion of magnesium sulfate, ketamine, and dexmedtomidine was used to maintain anesthesia. Opioids were used sparingly: we administered an average of 200 mcg of Fentanyl in 23 of 31 patients. Sugammadex was used to reverse neuromuscular blockade. Patients were extubated and transferred to PACU where capnography traces were continuously recorded using a Microstream Smart CapnoLine® Plus O2 Sampling Line (Medtronic: Dublin, Ireland) and IntelliVue MX700 patient monitor (Philips: Amsterdam, Netherlands) during recovery. Aggregate monitor displayed ETCO2 values were averaged over 30 sec and recorded at 5 min, 30 min, and 2 hours after admission to PACU. Any hypercapnia events, respiratory arrhythmias, or respiratory complications were noted. Patients were monitored for a minimum of two hours post-operatively. Patients reporting persistent pain with a VAS-pain score >4 received titrated hydromorphone IV PRN.
Results: No adverse respiratory events were noted and PACU respiratory measures were within normal limits, although several patients received supplemental oxygen (Table 2). Analysis of variance did not detect significant differences in ETCO2, SPO2, RR, or pain across the duration of the PACU stay.
Discussion: Patients undergoing bariatric surgery present a unique risk for pulmonary complications such as hypoventilation, hypercapnia, and apnea, in addition to possibly desaturation. Two-thirds of study subjects carried an OSA diagnosis and the rest were marked high risk for developing postoperative apnea. However, none of our patients experienced any adverse respiratory events, which may be attributed to a number of factors, including the sparing use of opioid during anesthesia and in PACU.
Capnography gives healthcare providers a prompt access to additional respiratory measures such as ETCO2, breathing rhythm, periodic apnea, and respiratory rate that are not otherwise available through pulse oximetry or tracheal acoustic monitoring. These measurements provide a more thorough assessment of the ventilation status of patients during recovery and allow providers to maintain high patient safety.
References:
[1] Pouwels S. et al.: Respir Med. 2016;117:73-80.
[2] Fu ES et al.: Chest J. 2004;126:1552–1558.
Table 1:
Table 2: