2020 FSA Posters
P002: REPEATING LACTATE CONCENTRATIONS IN WARD PATIENTS ADMITTED WITH A DIAGNOSIS OF POSSIBLE SEPSIS LACKS UTILITY FOR PREDICTING ESCALATION OF CARE OR MORTALITY
Jose Navas, MD; Richard Epstein, MD; Roman Dudaryk, MD; University of Miami
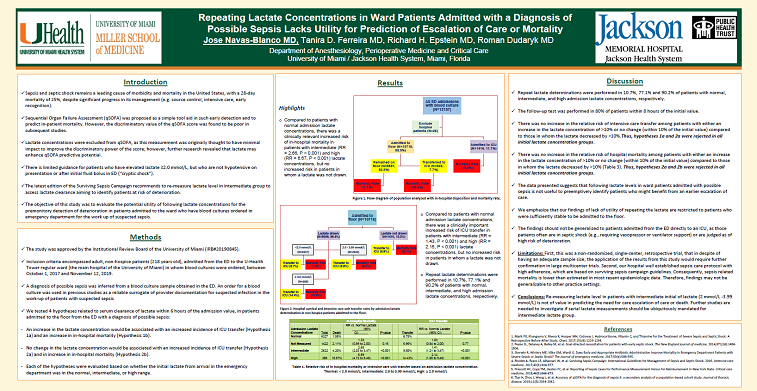
Introduction: Sepsis remains a major public health concern with a 28-day mortality of exceeding 25%. Early identification of patients at risk for sepsis and septic shock becomes crucial for timely initiation of treatment and appropriate disposition. Lactate may predict in-hospital mortality in patients with suspected sepsis, including those who are hemodynamically stable (cryptic shock). The objective of this study was to evaluate the utility of following lactate concentrations for the premonitory detection of deterioration in patients admitted to the ward who have blood cultures ordered in emergency department (ED) for the work up of suspected sepsis.
Methods: We performed a single-center, retrospective, cohort analysis of patient admitted to the ED of the University of Miami Hospital from October 2017 to November 2019. Inclusion criteria: adult patients (>18 years old) in whom blood cultures were ordered (as surrogate to identify those with suspected infection), identified through the electronic medical record. Exclusion criteria: pediatric patients, death in the ED, and hospice patients. We tested the following hypotheses: an increase in the lactate concentration would be associated with an increased incidence of ICU transfer (Hypothesis 1a) and an increase in in-hospital mortality (Hypothesis 1b). No change in the lactate concentration would be associated with an increased incidence of ICU transfer (Hypothesis 2a) and in increase in in-hospital mortality (Hypothesis 2b).
Results: During the study interval, 12157 patients were admitted to the hospital in whom a blood culture was obtained in the ED; 25 hospice patients were excluded from the analysis. Of the remaining 12132 patients, 1416 (11.7%) were initially admitted to an ICU and 10716 (88.3%) were admitted to a floor bed (Figure 1). Among the 10716 patients admitted initially to a floor bed with a blood culture drawn in the ED, baseline lactate determinations were performed in 86.8% (Figure 2). Compared to patients with normal admission lactate concentrations, there was a clinically relevant increased risk of in-hospital mortality in patients with intermediate (RR = 2.66, P < 0.001) and high (RR = 6.67, P < 0.001) lactate concentrations.
There was no increase in the relative risk of intensive care transfer among patients with either an increase in the lactate concentration of >10% or no change (within 10% of the initial value) compared to those in whom the lactate decreased by >10%. Thus, hypotheses 1a and 2a were rejected in all initial lactate concentration groups. There was no increase in the relative risk of hospital mortality among patients with either an increase in the lactate concentration of >10% or no change (within 10% of the initial value) compared to those in whom the lactate decreased by >10%. Thus, hypotheses 2a and 2b were rejected in all initial lactate concentration groups.
Conclusion: Re-measuring lactate level in patients with intermediate initial of lactate (2 mmol/L -3.99 mmol/L) is not of value in predicting the need for care escalation of care or death. Further studies are needed to investigate if serial lactate measurements should be ubiquitously mandated for intermediate lactate group.