2020 FSA Posters
P005: ANESTHESIA MANEUVERS TO DECREASE INTRAOCULAR PRESSURE RISE AFTER INTRAVITREAL INJECTION OF CHEMOTHERAPY IN CHILDREN WITH RETINOBLASTOMA
Marianna Martini, MD; Ana Mavarez, MD; Caroline Ripat, MD, MSPH; Alecia Stein, MD; University of Miami. Miller School of Medicine. Department of Anesthesiology, Perioperative Medicine and Pain Management.
Introduction: Retinoblastoma (Rb) is the most common primary intraocular malignancy in children1.Treatment of this disease was revolutionized with the initiation of intravitreal injection of chemotherapy (IViC) which improved outcomes due to its increased ocular penetration. However, this intervention contains some theoretical risk. IViC volume placed intravitreously is associated with significant acute increases in intraocular pressure (IOP)2. These fluctuations may cause injury to the optic nerve, retinal artery and most significantly led to speculation of extravasation of vitreal Rb cells to the extraocular space following needle penetration3. We hypothesized that anesthesia maneuvers may diminish or blunt acute IOP spike following IViC and present our preliminary data.
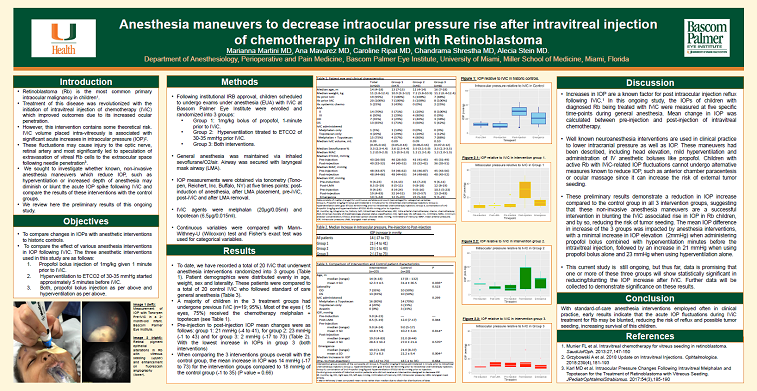
Methods: Following IRB approval, children with Rb scheduled to undergo exams under anesthesia with IViC at Bascom Palmer Eye Institute were enrolled and randomized into 1 of 3 groups. 1 mg/kg bolus of propofol bolus 1-minute prior to IViC (Group1); hyperventilation titrated to ETCO2 of 30-35 mmHg prior IViC (Group2); or both (Group3). General anesthesia was maintained via inhaled sevoflurane/O2/air. Airway was secured with laryngeal mask airway (LMA). IOP measurements were obtained via tonometry (Tono-pen, Reichert, Inc. Buffalo, NY) at five times: post-induction, after LMA placement, pre-iViC, post-iViC and after LMA removal. IViC agent/dose/volume were bevacizumab (1.25mg/0.05ml), melphalan (20μg/0.05ml) and topotecan (6.5μg/0.015ml). Continuous variables were compared with student’s two sample t-test and Pearson’s chi-square test. Fisher’s exact test was used for categorical variables.
Results: To date, a total of 18 IViCs have been included. Group 1(n=7), group 2(n= 3) and group 3(n=8). Patient’s demographics were distributed evenly in age, weight, sex and laterality. The majority of children had previous IViC (n=7;94%). 12 eyes (66%) received melphalan+topotecan (Table1). Comparing pre-injection to post-injection IOPs mean changes were as follows: Group1: 21mmHg (-4to73), for group2: -1mmHg (-1to33) and for group3: 2mmHg (-17to73) (Table2).
Discussion/Conclusion: Children with active Rb with IViC-related IOP fluctuations cannot undergo alternative measures known to reduce IOP, such as anterior chamber paracentesis or ocular massage since it can increase the risk of external tumor seeding. Anesthesia interventions exist which are known to lower intracranial pressures and IOP, accordingly. These maneuvers include Trendelenburg position; propofol bolus and mild hyperventilation. Our preliminary data suggest that these maneuvers may help to blunt the IViC associated rise in IOP in children. The mean IOP increase in the 3 groups was impacted by our interventions. Group2 demonstrated the largest blunting of IOP fluctuation, with post-IViC IOP essentially unchanged (Graph2), Group3 also, combining propofol bolus with hyperventilation with median elevation in IOP of 2mmHg (-17 to 73). These results suggest that with standard-of-care intervention employed often in anesthesia practice, we may be able to blunt the acute IOP fluctuation during IViC treatment for RB, making the procedures safer in these children.
References:
1. Munier FL et al. Intravitreal chemotherapy for vitreus seeding in retinoblastoma. SaudiJofOph.2013:27,147-150
2. Grzybowski A et al. 2018 Update on Intravitreal Injections. Ophtalmologica.2018:239(4),181-193
3. Karl MD et al. Intraocular Pressure Changes Following Intravitreal Melphalan and Topotecan for the Treatment of Retinoblastoma with Vitreous Seeding. JPediatrOphtalmolStrabismus.2017:54(3),185-190
.png)

.JPG)
.JPG)