2020 FSA Posters
P006: DETERMINATION OF GASTRIC EMPTYING TIMES FOR ORANGE JUICE IN HEALTHY INDIVIDUALS WITH USE OF BEDSIDE GASTRIC ULTRASOUND
Sindhuja R Nimma, MD; Linda Le-Wendling, MD; University of Florida
Introduction: Pulmonary aspiration of gastric content is a major anesthetic-related complication. Although current npo guidelines do not guarantee any specific outcome, verifying patient compliance is prudent. Point of care ultrasound can help differentiate an empty stomach from one with liquid/solid content. In 2011, “Bedside ultrasound assessment of gastric content” published in Canada described the sonographic characteristics of the gastric antrum. Based on ultrasound technique and calculations of gastric antrum cross-sectional area (CSA), the paper described a quick and non-invasive way to qualitatively and quantitatively evaluate gastric content. Most of this work was done with water and apple juice with limited evidence on emptying times of orange juice.
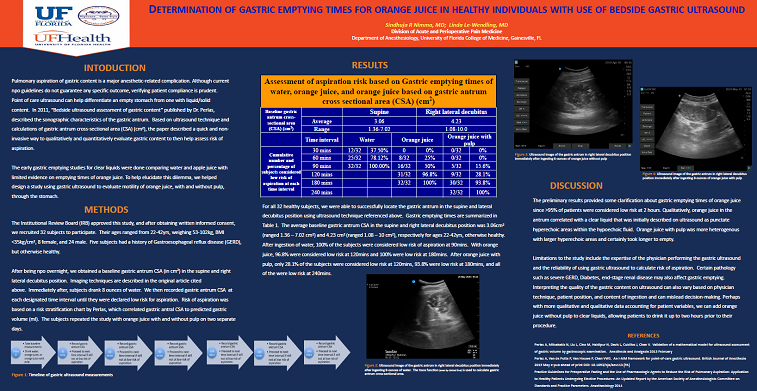
Methods: Following IRB approval and informed consent, we recruited 25 subjects (target goal 50) to participate. After being npo overnight, we obtained a baseline gastric antrum CSA (in cm2) in the supine and right lateral decubitus position. Imaging techniques are described in the original article cited above. Immediately after, subjects drank 8 ounces of water. We then recorded gastric antrum CSA every 30-minutes until they were declared low risk for aspiration. Risk of aspiration was based on a risk stratification chart by Perlas, which correlated gastric antral CSA to predicted gastric volume (ml). The subjects repeated the study with orange juice with and without pulp on two separate days.
Results: Of the 25 patients enrolled thus far, three had GERD but otherwise healthy and their ages ranged from 27 to 44 years. The average baseline antrum CSA was 3.07cm2 (ranged1.36-7.02cm2) and 4.59cm2 (ranged 1.08 – 10 cm2) in the supine and right lateral decubitus position, respectively. Of the 25 subjects, 96% were considered low risk of aspiration two hours after drinking orange juice. One patient, despite being healthy, was not considered low risk until 3 hours. After ingesting of orange juice with pulp, only 36% of the patients were considered low risk at 2 hours. In the water group, 84% of patients were low risk at 60min and 100% were low risk at 2 hours.
Discussion: The preliminary results provided some clarification about gastric emptying times of orange juice since >95% of patients were considered low risk at 2 hours. Qualitatively, orange juice in the antrum correlated with a clear liquid that was initially described on ultrasound as punctate hyperechoic areas within the hypoechoic fluid. Orange juice with pulp was more heterogenous with larger hyperechoic areas and certainly took longer to empty.
Limitations to the study include the expertise of the physician performing the gastric ultrasound and the reliability of using gastric ultrasound to calculate risk of aspiration. Certain pathology such as severe GERD, Diabetes, end-stage renal disease may also affect gastric emptying. Interpreting the quality of the gastric content on ultrasound can also vary based on physician technique, patient position, and content of ingestion and can mislead decision-making. Perhaps with more qualitative and qualitative data accounting for patient variables, we can add orange juice without pulp to clear liquids, allowing patients to drink it up to two hours prior to their procedure.