2020 FSA Posters
P007: RISK FACTORS ASSOCIATED WITH ATRIAL FIBRILLATION AFTER LIVER TRANSPLANTATION: A SINGLE CENTER RETROSPECTIVE STUDY
Nathalia Torres Buendia, MD; Fouad Souki, MD; Yehuda Raveh, MD; Vadim Shatz, MD; Joshua Livingstone, MD; Shashidhar Manchegowda, MD; Rofayda Gad, MD; Mohammad Khan, MD; Ramona Nicolau-Raducu, MD; University of Miami/Jackson Memorial Hospital
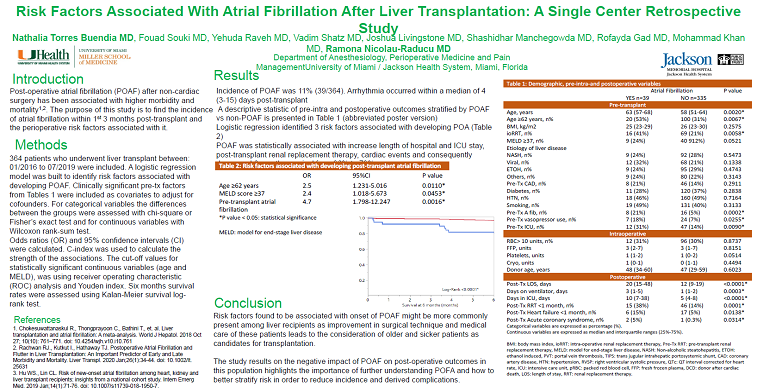
Introduction: Post-operative atrial fibrillation (POAF) after non-cardiac surgery has been associated with higher morbidity and mortality. Patients with liver disease undergoing liver transplantation seem to have a greater incidence of POAF. Risk factors for developing POAF and impact on post-operative outcomes for this patient population remain poorly characterized. The purpose of this study is to find the incidence of atrial fibrillation within 1st 3 months post-transplant and the perioperative risk factors associated with it.
Methods: 364 patients who underwent liver transplant between: 01/2016 to 07/2019 were included. Categorical variables were expressed as percentage (%) and differences between the groups were assessed with chi-square or Fisher’s exact test when appropriate. Continuous variables were expressed as median and interquartile ranges (25%-75%) and differences between the groups assessed with Wilcoxon rank-sum test. A logistic regression model was built to identify risk factors associated with developing POAF. Clinically significant pre-transplant factors from Table 1 were included as covariates to adjust for cofounders. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. C-index was used to calculate the strength of the associations. The cut-off values for statistically significant continuous variables (age and MELD), was using receiver operating characteristic (ROC) analysis and Youden index.
Results: Incidence of POAF was 11% (39/364). Arrhythmia occurred within a median of 4 (3-15) days post-transplant. A descriptive statistic of pre-intra and postoperative outcomes stratified by POAF vs non-POAF is presented in Table 1. Logistic regression identified 3 risk factors associated with developing POAF: recipient age≥62 years, MELD score ≥37 and history of pre-transplant atrial fibrillation (Table 2). The whole model was statistically significant (χ2=22.6, P<0.0001), and a C-index of 0.70 was calculated for these risk factors. A misclassification rate of 10% was calculated which reflect its ability to predict POAF in 90 of 100 recipients. POAF was statistically associated with increase length of hospital and ICU stay, post-transplant renal replacement therapy, cardiac events and consequently decreased 6-months survival.
Conclusion: Risk factors found to be associated with onset of POAF (age > 62 years old, MELD score >37, and previous history of atrial fibrillation) might be more commonly present among liver recipients as improvement in surgical technique and medical care of these patients leads to the consideration of older and sicker patients as candidates for transplantation. The study results on the negative impact of POAF on post-operative outcomes in this population highlights the importance of further understanding POAF and how to better stratify risk in order to reduce incidence and derived complications.

.PNG)
.JPG)