2020 FSA Posters
P010: PERIOPERATIVE RISK FACTORS ASSOCIATED WITH DELAYED GRAFT FUNCTION FOLLOWING DECEASED DONOR KIDNEY TRANSPLANTATION: A RETROSPECTIVE, SINGLE CENTER STUDY
Shashidhar Manchegowda, MD; Nicholas V Mendez; Nathalia Torres Buendia; Rofayada Gad; Mohammad Khan; Vadim Shatz; Joshua Livingstone; Fouad Souki; Yehuda Raveh; Ramona Nicolau- Raducu; Jackson Memorial Hospital
Introduction: Kidney transplantation is the therapy of choice for patients with end stage renal disease with superior survival and quality of life over dialysis. With an emphasis on the use of higher risk donor organs in the setting of increasingly higher risk recipients, a need exists for the identification of modifiable risk factors associated with poor outcomes. The aim of this analysis is to identify perioperative risk factors associated with delayed graft function (DGF).
Methods: All consecutive adult patients who underwent a deceased donor kidney transplant at our institution between January 2016 and July 2017 were identified with a final study population of 294 patients. All recipient and donor data was obtained from retrospective review of the electronic medical record and the United Network for Organ Sharing DonorNet® database. All donor kidneys were placed on hypothermic machine perfusion (HMP) pumps with the RM3 Renal Preservation Machine (Waters Instruments Inc. Rochester, MN). The primary outcome evaluated was the occurrence of DGF, defined as the need for dialysis within seven days of transplantation.
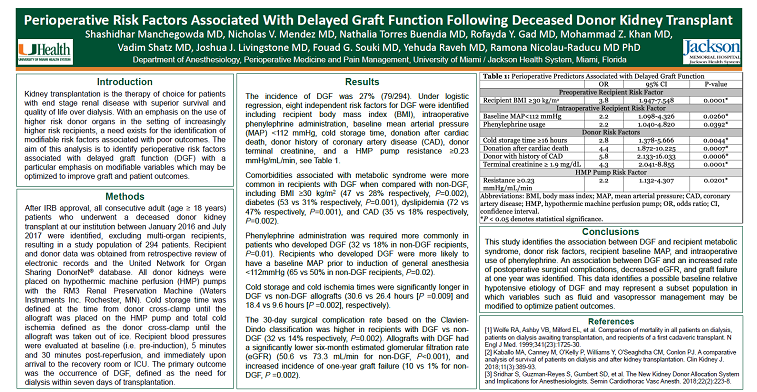
Results: The incidence of DGF was 27% (79/294). Under logistic regression, eight independent risk factors for DGF were identified including recipient body mass index (BMI), intraoperative phenylephrine administration, baseline mean arterial pressure (MAP) <112 mmHg, cold storage time, donation after cardiac death, donor history of coronary artery disease (CAD), donor terminal creatinine, and a HMP pump resistance ≥0.23 mmHg/mL/min, see Table 1. Comorbidities associated with metabolic syndrome were more common in recipients with DGF when compared with non-DGF, including BMI ≥30 kg/m2 (47 vs 28% respectively, P=0.002), diabetes (53 vs 31% respectively, P=0.001), dyslipidemia (72 vs 47% respectively, P=0.001), and CAD (35 vs 18% respectively, P=0.002). Phenylephrine administration was required more commonly in patients who developed DGF (32 vs 18% in non-DGF recipients, P=0.01). Recipients who developed DGF were more likely to have a baseline MAP prior to induction of general anesthesia <112mmHg (65 vs 50% in non-DGF recipients, P=0.02). Cold storage and cold ischemia times were significantly longer in DGF vs non-DGF allografts (30.6 vs 26.4 hours [P =0.009] and 18.4 vs 9.6 hours [P =0.002], respectively). The 30-day surgical complication rate based on the Clavien-Dindo classification was higher in recipients with DGF vs non-DGF (32 vs 14% respectively, P=0.002). Allografts with DGF had a significantly lower six-month estimated glomerular filtration rate (eGFR) (50.6 vs 73.3 mL/min for non-DGF, P<0.001), and increased incidence of one-year graft failure (10 vs 1% for non-DGF, P =0.002).
Conclusions: This study identifies the association between DGF and recipient metabolic syndrome, donor risk factors, recipient baseline MAP, and intraoperative use of phenylephrine. An association between DGF and an increased rate of postoperative surgical complications, decreased eGFR, and graft failure at one year was identified. This data identifies a possible baseline relative hypotensive etiology of DGF and may represent a subset population in which perioperative variables such as fluid management and vasopressor administration may be modified to optimize patient outcomes, particularly in the setting of high-risk recipients and donor organs.

.JPG)