2020 FSA Posters
P011: HEART FAILURE FOLLOWING LIVER TRANSPLANTATION: A RETROSPECTIVE SINGLE CENTER EXPERIENCE
Rofayda Gad; Fouad Souki; Mohammad Z Khan; Shashidhar Manchegowda; Nathalia Torres Buendia; Ramona Nicolau-Raducu; Miami University, Jackson Memorial Hospital
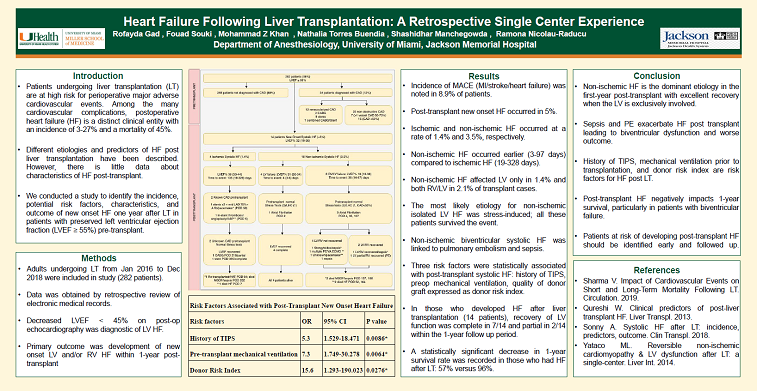
Introduction: Patients undergoing liver transplantation (LT) are at high risk for perioperative major adverse cardiovascular events (MACE) despite thorough preoperative cardiac evaluation [1]. Among the many cardiovascular complications, postoperative heart failure (HF) is a distinct clinical entity with an incidence of 3-27% and a mortality of 45% [2,3].Different etiologies and predictors of HF post liver transplantation have been described [2-4]. However, there is paucity of data about characteristics of HF post-transplant. We conducted a study to identify the incidence, potential risk factors, characteristics, and outcome of new onset HF one year after LT in patients with preserved left ventricular ejection fraction pre-transplant.
Methods: Following institutional review committee approval, liver transplants performed from January 2016 to December 2018 in patients ≥18 years old at University of Miami/Jackson Memorial Hospital were reviewed. 282 patients were included in the study. Perioperative data was obtained by retrospective review of electronic medical records. Logistic regression using a stepwise personality, with a stopping rule P-value threshold of 0.25 for probability to enter, and a more stringent P-value of 0.10 for probability to leave conducted in mixed directions, was performed to identify predictors statistically associated with HF within first year post-transplant. Clinically significant (P<0.100) of the recipient & donor variables were entered into a multivariable analysis; Odds ratios and 95% Confidence Interval (CI) were calculated, and a C-index was calculated to measure the strength of the associations. The bootstrap method for 2500 iterations yielded bias-corrected C-index and 95% CI for the regression coefficients of the final model. Survival was estimated with Kaplan-Meier survival method. All statistical analyses were performed with JMP 14.
Results: The incidence of MACE (MI/stroke/heart failure) was noted in 8.9% (25/282) of patients. Post-transplant new onset HF occurred in 5% (14/282). Ischemic and non-ischemic HF occurred at a rate of 1.4% (4/282) and 3.5% (10/282), respectively (Figure 1). Non-ischemic HF comprised 71% (10/14) of post-transplant HF cases and occurred at an earlier date (3-97 days) compared to ischemic HF (19-328 days) (Figure 1). The most likely etiology for non-ischemic isolated LV HF was stress-induced; all these patients survived the event. Three risk factors were statistically associated with post-transplant new onset systolic HF: history of TIPS, mechanical ventilation prior transplantation, and quality of the donor graft expressed as donor risk index (DRI) (Table 1). In those who developed HF after liver transplantation (14patients), recovery of LV function was complete in 7/14 and partial in 2/14 within the 1-year follow up period. When comparing patients with and without post-transplant systolic new onset HF, a statistically significant decrease in 1-year survival rate was recorded: 57% versus 96% (Figure 2).
Conclusion: Non-ischemic HF is the dominant etiology in the first-year post-transplant with excellent recovery when the LV is exclusively involved. History of TIPS, mechanical ventilation prior to transplantation, and donor risk index were identified as risk factors for development HF post LT. Post-transplant HF negatively impacts 1-year survival rate, particularly in patients with biventricular failure. Patients at risk of developing post-transplant HF should be identified early and followed up carefully.