2020 FSA Posters
P012: SIMULATION USE IN THE OUTREACH SETTING: A NOVEL APPROACH TO BUILDING SUSTAINABILITY
Marie Nader, MD1; Gulsen Tasdelen-Teker, PhD2; Anthony DeStephens, MSME1; Samsun Lampotang, PhD1; Irina Prelipcean, MD1; Robert Smith, MD1; William Bortcosh, MD1; Nicolas Chiriboga Salazar, MD1; Natalia Martinez Schlurmann, MD1; Usama Hamdan, MD3; Jennifer Munoz Pareja, MD1; 1University of Florida; 2Hacettepe University; 3Global Smile Foundation
Background: Simulation is a well-studied teaching tool for multi-disciplinary teamwork, crisis resource management and communication skills. These elements are essential for successful international medical missions which include health care providers with different areas of expertise, levels of training, or familiarity with the outreach setting and each other’s roles. The Global Smile Foundation, a non-profit organization that provides free comprehensive care to children with congenital facial deformities in the Middle East, North Africa, and South America, has previously developed and implemented safety checklists and emergency response protocols. This has resulted in improved mission logistics and refined patient safety mechanisms. However, the effect of immersive simulation on team dynamics remains poorly studied in similar settings. With that in mind, we hypothesize that incorporating simulation into the workflow of international medical missions will result in enhanced team preparedness for addressing the innate challenges of working in the outreach setting.
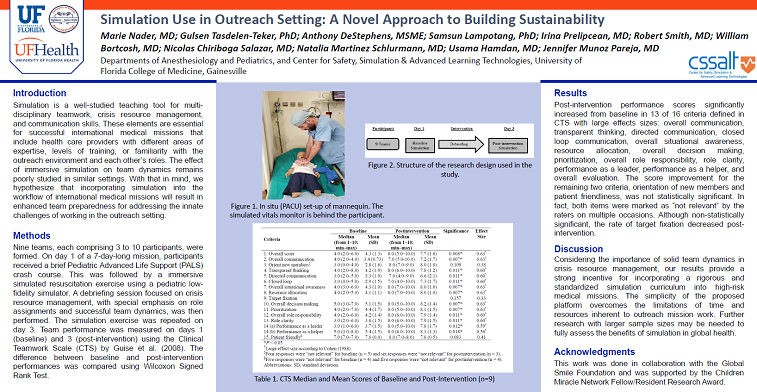
Methods: We used a one-group pre-intervention/post-intervention quasi-experimental design to measure the effectiveness of simulation training in improving overall team performance during patient resuscitation. Both visiting and hosting board certified health care providers and trainees in pediatrics, pediatric anesthesiology, surgery and nursing were included in our study. Medical and graduate students who have not started their internship or residency training or individuals with poor fluency in English were excluded. A total of nine teams, each composed of 3 to 10 participants were formed. On day 1 of a 7 day long mission, participants received a brief crash course focusing on major PALS algorithms. This was followed by a simulated resuscitation exercise using a pediatric low fidelity simulator. A debriefing session focused on crisis resource management, with special emphasis on role assignments and successful team dynamics was then performed. The simulation exercise was repeated on day 3. Team performance was measured on both day 1 (baseline) and day 3 (post-intervention) using the Clinical Teamwork Scale (CTS) by Guise et al. (2008). The difference between baseline and post-intervention performances was compared using Wilcoxon Signed Rank Test.
Results: Post-intervention performance scores significantly increased from baseline in 13 out of 16 criteria defined in CTS with large effects sizes: overall communication, transparent thinking, directed communication, closed loop communication, overall situational awareness, resource allocation, overall decision making, prioritization, overall role responsibility, role clarity, performance as a leader, performance as a helper and overall evaluation. The score improvement for the remaining two criteria, orientation of new members and patient friendliness, was not statistically significant. In fact, both items were marked as “not relevant” by the raters on multiple occasions. Although non statistically significant, the rate of target fixation decreased post-intervention.
Conclusion: Considering the importance of solid team dynamics in crisis resource management, our results provide a strong incentive for incorporating a rigorous and standardized simulation curriculum into high-risk medical missions. The simplicity of the proposed platform overcomes the limitations of time and resources inherent to outreach mission work. Further research with larger sample sizes may be needed to fully assess the benefits of simulation in global health.