2020 FSA Posters
P093: COMPARISON OF INTERSCALENE VS. CERVICAL PARAVERTEBRAL CONTINUOUS NERVE BLOCK FOR SHOULDER ARTHROPLASTY
Phuong Bui, MD1; Maha Balouch, MA2; Garrett Enten, BS2; Suvikram Puri, MD1; Enrico M Camporesi, MD2; 1Division of Acute Pain Medicine, TEAMHealth Anesthesia; 2TEAMHealth Anesthesia Research
Introduction: A continuous brachial plexus block can be used for major surgical procedures involving the shoulder. We compared the analgesic efficacy of the Interscalene approach (IS) to the Cervical Paravertebral approach (CPV) for elective primary shoulder arthroplasty.
Methods: The University of South Florida IRB approved this retrospective chart review.
IS block was completed in the sitting position. Ultrasound was used to identify the brachial plexus at the interscalene level. After local infiltration with 1% Lidocaine, a 17G Tuohy needle was inserted using an in-plane approach. 20ml of 0.5% Ropivacaine were injected after negative aspiration and appropriate local anesthetic spread was observed. A 19G continuous nerve block catheter was then inserted and proper placement was confirmed via ultrasound.
CPV block was completed in the lateral decubitus position. Local infiltration with 1% Lidocaine was performed; a 17G Tuohy needle was inserted in the groove between the anterior border of the trapezius muscle and the posterior border of the levator scapulae muscle. The C7 transverse process was contacted and the needle was advanced laterally and anteriorly at a 30 degree angle while aiming towards the suprasternal notch. A nerve stimulator was used to elicit a C6 nerve root response in form of a biceps muscle twitch. A 19G continuous nerve block catheter was threaded while maintaining the biceps muscle twitch response. Additional confirmation of correct catheter location was obtained via the Raj test. 20ml of 0.5% Ropivacaine were injected through the catheter after negative aspiration.
Surgery was subsequently completed under general anesthesia. CPV blocks were all performed by a single physician (SP); Interscalene blocks were done by different providers under supervision of SP during the same 3 month time period. A continuous catheter infusion was maintained throughout the surgical procedure and post-operative days (POD) 1 and 2. The infusion rate was 0.2% Ropivacaine at 0.5 mL/hr plus 2.5 mL bolus every 30 minutes, up to a maximum of 10 mL/hr. We measured duration of continuous infusion and total postoperative Morphine Milligram Equivalent (MME) from chart revue and from patient requests during two postoperative days.
Statistical comparison within groups was completed with paired t-test; Cohen’s d was calculated for POD 2 comparison between the two types of blocks.
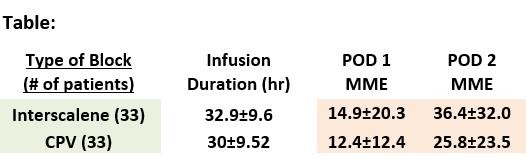
Results: The table summarizes MME requested by patients POD 1 to POD 2; the duration of continuous block infusion was similar in both cases (all values are Mean±SD).
Consistently, both patient groups required significantly more MME on POD 2 vs. POD 1 (p<0.01 by paired t-test); on POD 2 we noticed a slight reduction of MME in the CPV group compared to the IS group which did not reach statistical significance but shows a medium effect size (Cohen’s d=0.38). The postoperative local anesthesia efficacy appears reduced on POD 2 for IS block.
Discussion/Conclusion: Both IS and CPV approaches to brachial plexus block can be well-suited for primary shoulder arthroplasty. Both types of approach were well-tolerated and there were no major complications.