2021 FSA Posters
P001: INTRACARDIAC THROMBOSIS DURING LIVER TRANSPLANTATION: A 22-YEAR SINGLE-INSTITUTION STUDY
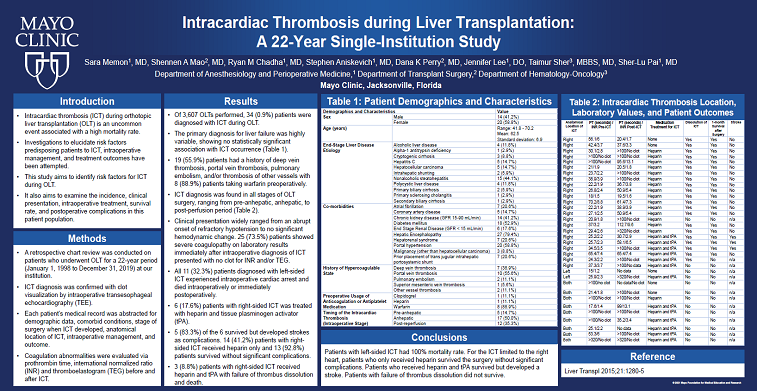
Sara Memon, MD; Shennen A Mao, MD; Ryan M Chadha, MD; Stephen Aniskevich, MD; Dana K Perry, MD; Jennifer Lee, DO; Taimur Sher, MBBS, MD; Sher-Lu Pai, MD; Mayo Clinic
INTRODUCTION: Intracardiac thrombosis (ICT) during orthotopic liver transplantation (OLT) is an uncommon event associated with a high mortality rate. Investigations to elucidate risk factors predisposing patients to ICT, intraoperative management, and treatment outcomes have been attempted. This study aims to identify risk factors for ICT during OLT. It also aims to examine the incidence, clinical presentation, intraoperative treatment, survival rate, and postoperative complications in this patient population
METHOD: A retrospective chart review was conducted on patients who underwent OLT for a 22-year period (January 1, 1998 to December 31, 2019) at our institution. ICT diagnosis was confirmed with clot visualization by intraoperative transesophageal echocardiography (TEE). Each patient’s medical record was abstracted for demographic data, comorbid conditions, stage of surgery when ICT developed, anatomical location of ICT, intraoperative management, and outcome. Coagulation abnormalities were evaluated via prothrombin time, international normalized ratio (INR) and thromboelastogram (TEG) before and after ICT.
RESULTS: Of 3,607 OLTs performed, 34 (0.9%) patients were diagnosed with ICT during OLT. The primary diagnosis for liver failure was highly variable, showing no statistically significant association with ICT occurrence (Table 1). 19 (55.9%) patients had a history of deep vein thrombosis, portal vein thrombosis, pulmonary embolism, and/or thrombosis of other vessels with 8 (88.9%) patients taking warfarin preoperatively. ICT diagnosis was found in all stages of OLT surgery, ranging from pre-anhepatic, anhepatic, to post-perfusion period (Table 2). Clinical presentation widely ranged from an abrupt onset of refractory hypotension to no significant hemodynamic change. 25 (73.5%) patients showed severe coagulopathy on laboratory results immediately after intraoperative diagnosis of ICT presented with no clot for INR and/or TEG. All 11 (32.3%) patients diagnosed with left-sided ICT experienced intraoperative cardiac arrest and died intraoperatively or immediately postoperatively. 6 (17.6%) patients with right-sided ICT was treated with heparin and tissue plasminogen activator (tPA). 5 (83.3%) of the 6 survived but developed strokes as complications. 14 (41.2%) patients with right-sided ICT received heparin only and 13 (92.8%) patients survived without significant complications. 3 (8.8%) patients with right-sided ICT received heparin and tPA with failure of thrombus dissolution and death.
CONCLUSIONS: A previous history of vascular thrombosis may be a risk factor for ICT development during OLT. Patients with left-sided ICT had 100% mortality rate. Patients with right-sided ICT, who only received heparin, survived surgery and did not have significant complications. Patients with right-sided ICT, who received heparin and tPA, survived but developed a stroke. Patients with right-sided ICT, with failure of thrombus dissolution despite heparin and tPA, did not survive surgery. Intraoperative TEE placement was used to diagnose ICT in all cases but was mostly done emergently during cardiopulmonary instability as opposed to routinely at the beginning of surgery. Use of tPA as the treatment of ICT may increase risk of stroke. Postoperative brain imaging may be useful to rule out stroke when tPA or heparin is used intraoperatively to facilitate prompt diagnosis. Additional study to compare ICT patients with matching cohort may provide a better understanding of risk factors.
REFERENCE: Liver Transpl 2015;21:1280-5
.jpg)
.jpg)