2021 FSA Posters
P006: PERIOPERATIVE MANAGEMENT OF A PATIENT WITH OPIOID USE DISORDER AND ACUTE LOWER EXTREMITY LIMB ISCHEMIA
Gianfranco Molfetto, DO; Taimoor Khan, MD; Onassis Naim; Nick Davies, AA; Veronica Montes-Berrios, MD; Nancy Erickson, MD; Memorial Healthcare System
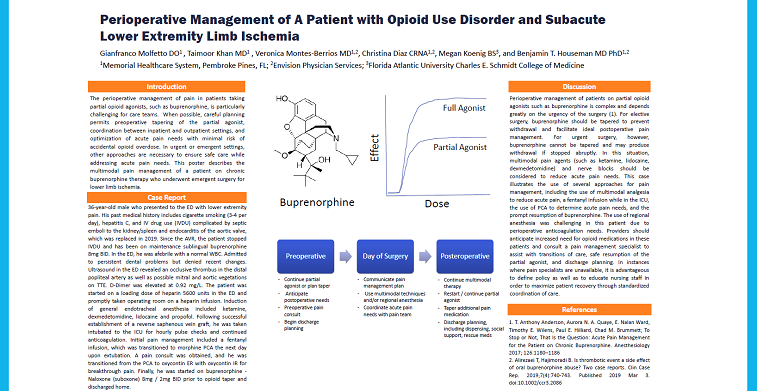
Introduction: Perioperative management of patients on partial opioid agonists such as buprenorphine is complex and depends greatly on the urgency of the surgery (1-3). For elective surgery, buprenorphine should be tapered to prevent withdrawal and facilitate postoperative pain management. For urgent or emergent surgery, buprenorphine cannot be tapered and may produce withdrawal if abruptly stopped. This case report describes the perioperative pain management of an opioid use disorder patient with acute lower extremity limb ischemia.
Case Description: A 36 yo male presented to the emergency department with complaints of lower extremity pain. His past medical history was significant for cigarette smoking (3-4 per day), hepatitis C, and intravenous drug use complicated by septic emboli to the kidney / spleen and endocarditis of the aortic valve, which was replaced in 2019. Since the AVR, the patient has stopped IVDU and was on maintenance sublingual buprenorphine 8mg BID. In the ED, he was afebrile with a normal white blood count. He did note persistent dental problems, but did not endorse recent changes.
Ultrasound in the ED revealed an occlusive thrombus in the distal popliteal artery as well as possible mitral and aortic vegetations on TTE. A loading dose of heparin 5600 units was administered in the emergency department and the patient was taken to the operating room on a heparin infusion. Following induction of general endotracheal anesthesia with ketamine, dexmedetomidine, lidocaine and propofol, an arterial line and central line were placed. A reverse saphenous vein graft was established in a lengthy 6 hour procedure, and the patient was taken intubated to the ICU for pulse checks every hour and continued anticoagulation.
Postoperatively, a pain consult was obtained, a fentanyl infusion was begun in ICU, and the infusion was transitioned to morphine PCA when the patient was extubated the following day. A pain consult was obtained. Over the several days, he was transitioned from the PCA to oxycontin ER with oxycontin IR for breakthrough pain. Finally, he was started on buprenorphine - Naloxone (suboxone) 8mg / 2mg BID prior to opioid taper and discharge home with pre-arranged support, dispensing agreements, scheduled regular followup meetings, and rescue medication in case of overdose.
Discussion: Patients taking buprenorphine represent a significant perioperative challenge that requires coordinated planning, particularly in urgent surgeries where withdrawal may occur. This case illustrates the use of several approaches for pain management, including a fentanyl infusion while in the ICU, the use of PCA to determine opiate needs, the prompt resumption of buprenorphine, and the use of multimodal analgesia to reduce acute surgical pain. This case also illustrates the importance of coordinated post-discharge pain management planning that includes dispensing, monitoring, and caregiver support.
1. Anderson, T et al. Anesthesiology 2017; 126:1180–1186
2. S Kawatsu, et al The Annals of Thoracic Surgery, Volume 105, Issue 5, 2018, Pages 1316-1321
3. Leighton BL and Crock LW. Anesth Analg 2017: 125:1779-1783