2021 FSA Posters
P009: LAPAROSCOPIC BARIATRIC SURGERY IN PATIENT WITH CARDIOGENIC SHOCK FOR WEIGHT OPTIMIZATION PRIOR TO LVAD INSERTION
Jeremy Armbruster, MD; Paola Aranda-Valderrama, MD; Tatiana Jamroz, MD; Juan Botero, MD; Cleveland Clinic FLorida
Introduction: Left Ventricular Assist Devices (LVADs) can serve as a bridge-to-therapy in patients with heart failure who may be eligible for heart transplant. LVADs may also serve as destination therapy in patients with heart failure who are not eligible for a heart transplant. Morbid obesity can increase a patient’s risk for perioperative complications and is often considered a relative contraindication for heart transplantation. Here we present a patient with heart failure who underwent bariatric surgery with the intent for weight optimization prior to LVAD insertion.
Our patient is a 26-year-old male with combined systolic/diastolic heart failure (EF 15%) presumably due to alcohol abuse, pulmonary hypertension, and morbid obesity with a BMI of 50.4. The patient was maintained on a milrinone infusion at 0.25 mcg/kg/min, amiodarone for multiple episodes of ventricular tachycardia, and furosemide for fluid overload. He was presented to the Transplant/LVAD committee, which recommended laparoscopic bariatric surgery to cardiac surgery. In discussion with cardiology, an Impella CP® was inserted to help the patient better tolerate abdominal insufflation during laparoscopic surgery.
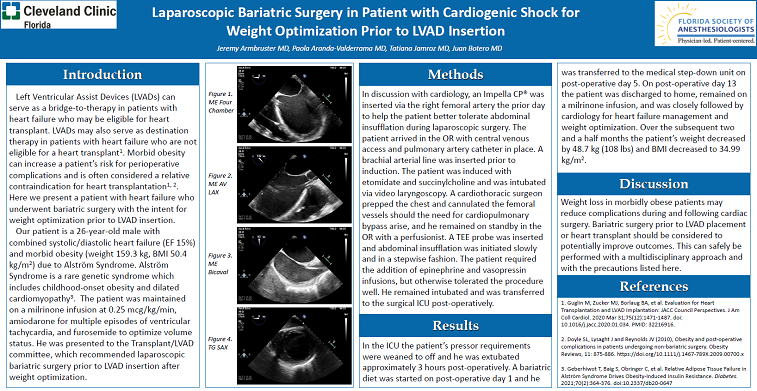
Methods: The patient arrived in the OR with central venous access and pulmonary artery catheter in place. A brachial arterial line was inserted prior to induction. The patient was induced with etomidate and succinylcholine and was intubated via video laryngoscopy. A cardiothoracic surgeon prepped the chest and cannulated the femoral vessels should the need for cardiopulmonary bypass arise, and he remained on standby in the OR with a perfusionist. A TEE probe was inserted and abdominal insufflation was initiated slowly and in a stepwise fashion. The patient required the addition of epinephrine and vasopressin infusions but otherwise tolerated the surgery well. He remained intubated and was transferred to the surgical ICU post-operatively.
Results: In the ICU the patient’s pressor requirements were weaned to off and he was extubated approximately 3 hours post-operatively. A bariatric diet was started on post-operative day 1 and transferred to the medical step-down unit on post-operative day 5. The patient will be discharged to home, remain on a milrinone infusion, and will be reevaluated for LVAD placement pending optimal weight loss.
Discussion: Weight loss in morbidly obese patients may reduce complications during and following cardiac surgery. Bariatric surgery prior to LVAD placement or heart transplant should be considered to potentially improve outcomes.