2021 FSA Posters
P010: CENTRAL LINE PLACEMENT - IS IT VENOUS OR ARTERIAL?
Karla M Objio, BA1; Angela Chang, MD2; Catalina Carvajal, DO2; Sofia Fischer, MD2; 1Kiran C Patel College of Osteopathic Medicine; 2HCA Healthcare East Florida Division GME/Kendall Regional Medical Center Program
Introduction/Background: Central venous access is indicated in situations that require rapid transfusion of blood products and/or hemodynamic monitoring. Here we present a case of a 67-year-old male with a history of uncontrolled hypertension who presented with complaints of flank pain for 2 hours. CT of the abdomen revealed an infrarenal 9 cm AAA with surrounding retroperitoneal hemorrhage of varying density, suggesting varying age.
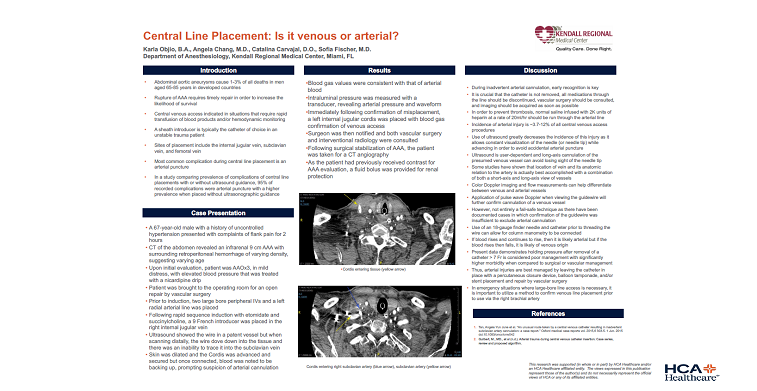
Methods: The patient was brought to the operating room for an open repair by vascular surgery. Following rapid sequence induction with etomidate and succinylcholine, a 9 French introducer was placed in the right internal jugular vein. Ultrasound was then used to confirm placement. However, while the wire appeared to be in a patent vessel, when scanning distally, the wire dove down into the tissue and there was an inability to trace it into the subclavian vein. The skin was dilated and the cordis was advanced and secured. Upon connecting to the hot line, blood was seen backing up and this prompted further evaluation.
Results: Upon connecting to the hot line, blood was seen backing up, immediately prompting suspicion of arterial cannulation. A sample of blood was taken, and blood gas values were consistent with that of arterial blood. Intraluminal pressure was measured with a transducer which revealed arterial pressure and waveform. Immediately following confirmation of misplacement, a left internal jugular cordis was placed with blood gas confirmation of venous access.
Discussion/Conclusion: The incidence of arterial injury is reported to be 3.7-12% of all central venous access procedures and the use of ultrasound greatly decreases the incidence of this injury. Ultrasound is user dependent and long-axis cannulation of the presumed venous vessel can avoid losing sight of the needle tip. Additionally, application of pulse wave doppler when viewing the guide wire will further confirm cannulation of a venous vessel. Using a small 18 gauge finder needle and catheter prior to threading the wire can allow for column manometry to be connected. If the blood rises and continues to rise, then it is likely arterial. On the other hand, if the blood rises then falls, it is likely of venous origin. Intervention by a vascular surgeon is indicated when an arterial injury is caused by a large bore needle, such as in this case. Arterial injuries can be managed safely and successfully by a vascular surgeon if the catheter is left in place with a percutaneous closure device, balloon tamponade, and/or stent placement. In emergency situations where large-bore line access is necessary, it is important to utilize a method to confirm venous line placement prior to use.