2021 FSA Posters
P011: SUCCESSFUL SEDATION OF A PATIENT WITH PREVIOUS TAKOTSUBO CARDIOMYOPATHY (BROKEN HEART SYNDROME) IN AN AMBULATORY SETTING
Lindsey Webb, BSME1; April Taniguchi, BS1; Oscar J Webb, MD, MA2; 1University of Central Florida; 2Brevard Physician Associates
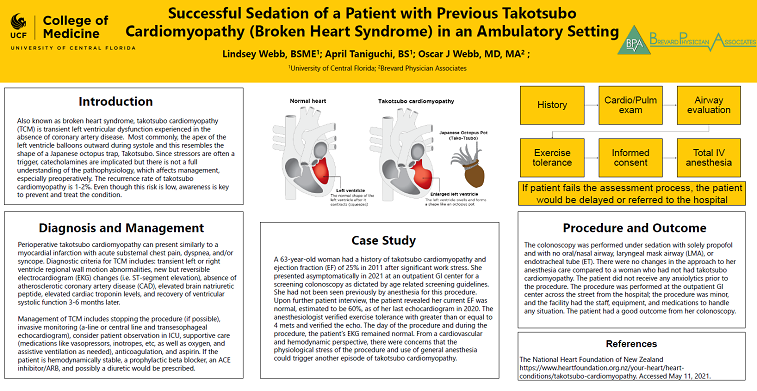
Also known as broken heart syndrome, takotsubo cardiomyopathy (TCM) is transient left ventricular dysfunction experienced in the absence of coronary artery disease. Most commonly, the apex of the left ventricle balloons outwards during systole and this resembles the shape of a Japanese octopus trap, Takotsubo. Since stressors are often a trigger, catecholamines are implicated but there is not a full understanding of the pathophysiology, which affects management, especially preoperatively. The recurrence rate of takotsubo cardiomyopathy is 1-2%. Even though this risk is low, awareness is key to preventing and treating the condition.
Perioperative takotsubo cardiomyopathy can present similarly to a myocardial infarction with acute substernal chest pain, dyspnea, and/or syncope. Diagnostic criteria for TCM includes: transient left or right ventricle regional wall motion abnormalities, new but reversible electrocardiogram (EKG) changes (i.e. ST-segment elevation), absence of atherosclerotic coronary artery disease (CAD), elevated brain natriuretic peptide, elevated cardiac troponin levels, and recovery of ventricular systolic function 3-6 months later.
Management of TCM includes stopping the procedure (if possible), invasive monitoring (a-line or central line and transesophageal echocardiogram), consider patient observation in ICU, supportive care (medications like vasopressors, inotropes, etc, as well as oxygen, and assistive ventilation as needed), anticoagulation, and aspirin. If the patient is hemodynamically stable, a prophylactic beta blocker, an ACE inhibitor/ARB, and possibly a diuretic would be prescribed.
A 63-year-old woman had a history of takotsubo cardiomyopathy and Ejection Fraction (EF) of 25% in 2011 after significant work stress. She presented asymptomatically in 2021 at an outpatient GI center for a screening colonoscopy as dictated by age related screening guidelines. She had not been seen previously by anesthesia for this procedure. Upon further patient interview, the patient revealed her current ejection fraction was normal, estimated to be 60%, as of her last echocardiogram in 2020. The day of the procedure and during the procedure, the patient’s EKG remained normal. From a cardiovascular and hemodynamic perspective, there were concerns that the physiological stress of the procedure and use of general anesthesia could trigger another episode of takotsubo cardiomyopathy.
The colonoscopy was performed under sedation with solely propofol and with no laryngeal mask airway (LMA). There were no changes in the approach to her anesthesia care compared to a woman who had not had takotsubo cardiomyopathy. The patient did not receive any anxiolytics prior to the procedure. The procedure was able to be performed at the outpatient GI center because the center was across the street from the hospital, the procedure was small, and the facility has the staff, equipment, and medications to handle any situation. The patient had a good outcome from her colonoscopy.