2021 FSA Posters
P012: PLATELET-RICH PLASMA FOR RHEUMATOID ARTHRITIS: A CASE SERIES
Dana Shively1; Neel Amin, MD2; 1Florida International University, Herbert Wertheim College of Medicine; 2University of Washington in Seattle
Background: Rheumatoid Arthritis (RA) is a chronic disease characterized by severe inflammation that leads to degradation of articular cartilage and the formation of bony erosions. Unfortunately, this condition affects about 5 in 1000 individuals worldwide, peaking in the sixth decade of life [1]. Today, anesthesiologist led pain management clinics have begun to take special consideration into the treatment of patients with RA as this progressive disease impairs work capacity and impacts a patient’s psychological state due to chronic pain [2,5]. We present clinical cases in which PRP was used for treatment of RA in patients seeking a new therapy to control their chronic disease.
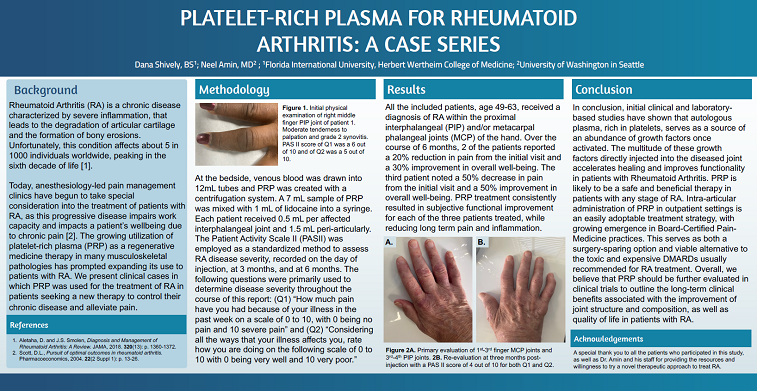
Methods: At the bedside, venous blood was drawn into 12mL tubes and PRP was created with a centrifugation system. A 7 mL sample of PRP was mixed with 1 mL of lidocaine into a syringe. Each patient received 0.5 mL per affected interphalangeal joint and 1.5 mL peri-articularly. The Patient Activity Scale II was employed as a standardized method to assess RA disease severity. Scores were recorded on the day of injection, at 3 months, and 6 months. The following questions were primarily used to determine disease severity throughout the course of this report: “How much pain have you had because of your illness in the past week on a scale of 0 to 10, with 0 being no pain and 10 being severe pain” and “Considering all the ways that your illness affects you, rate how you are doing on the following scale of 0 to 10, with 0 being very well and 10 being very poor.”
Results: All of the included patients, age 49-63, received a diagnosis of RA within the proximal interphalangeal and metacarpal phalangeal joints of the hand. Over the course of 6 months, 2 of the patients reported a 20% reduction in pain from the initial visit and a 30% improvement of overall well-being. The third patient noted a 50% decrease in pain from the initial visit and a 50% improvement in overall well-being. PRP treatment consistently resulted in functional improvement for each of the three patients treated, while reducing long term pain and inflammation.
Conclusion: In conclusion, initial clinical and laboratory-based studies have shown that autologous plasma-rich platelets serve as an abundant source of growth factors once activated. The multitude of these growth factors directly injected into the diseased joint accelerates healing and improves functionality in patients with RA. PRP is likely to be a safe and beneficial therapy in patients with any stage of RA. Intra-articular administration of PRP in outpatient settings is an easily adoptable treatment strategy, with growing emergence in our Board Certified Pain-Medicine practices. This serves as both a surgery sparing option and a viable alternative to the toxic and expensive DMARDs usually recommended for RA treatment. Overall, we believe that PRP should be further evaluated in clinical trials to outline the long-term clinical benefit in the improvement of joint structure and composition, as well as quality of life in patients with RA.