2021 FSA Posters
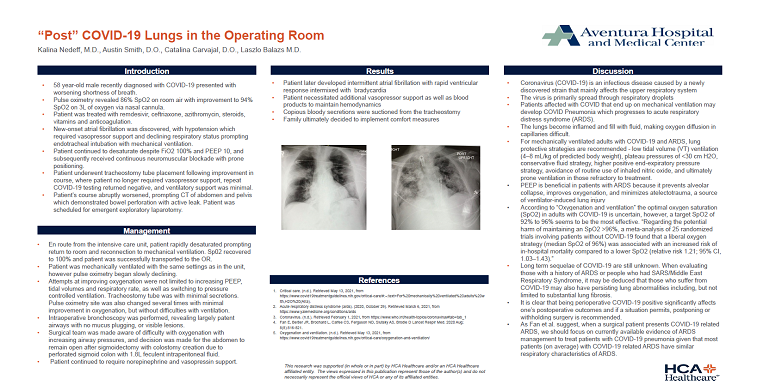
P018: "POST" COVID-19 LUNGS IN THE OPERATING ROOM
Kalina Nedeff, MD; Austin Smith, DO; Kendall Regional Medical Center
Introduction: 58 year-old male recently diagnosed with COVID-19 presented with worsening shortness of breath. Pulse oximetry revealed 86% SpO2 on room air with improvement to 94% SpO2 on 3L of oxygen via nasal cannula. Patient was treated with remdesivir, ceftriaxone, azithromycin, steroids, vitamins and anticoagulation. New-onset atrial fibrillation was discovered, with hypotension which required vasopressor support and declining respiratory status prompting endotracheal intubation with mechanical ventilation. Patient continued to desaturate despite FiO2 100% and PEEP 10, and subsequently received continuous neuromuscular blockade with prone positioning. Patient underwent tracheostomy tube placement following improvement in course, where patient no longer required vasopressor support, repeat COVID-19 testing returned negative, and ventilatory support was minimal. Patient’s course abruptly worsened, prompting CT of abdomen and pelvis which demonstrated bowel perforation with active leak. Patient was scheduled for emergent exploratory laparotomy.
Methods: En route from the intensive care unit, patient rapidly desaturated prompting return to room and reconnection to mechanical ventilation. Sp02 recovered to 100% and was successfully transported to the OR. Patient was mechanically ventilated with the same parameters as in the unit, however pulse oximetry began slowly declining. Attempts at improving oxygenation were not limited to increasing PEEP, tidal volumes and respiratory rate, as well as switching to pressure controlled ventilation. Tracheostomy tube was with minimal secretions. Pulse oximetry site was also changed several times with minimal improvement in oxygenation, but without difficulties with ventilation. Intraoperative bronchoscopy was performed, revealing largely patent airways with no mucus plugging, or visible lesions. Surgical team was made aware of difficulty with oxygenation with increasing airway pressures, and decision was made for the abdomen to remain open after sigmoidectomy with colostomy creation due to perforated sigmoid colon with 1.8L feculent intraperitoneal fluid. Patient continued to require norepinephrine and vasopressin support.
Results: Patient later developed intermittent atrial fibrillation with rapid ventricular response and bradycardia, and necessitated additional vasopressor support as well as blood products to maintain hemodynamics. Copious bloody secretions were suctioned from the tracheostomy. Family ultimately decided to implement comfort measures.
Discussion: Coronavirus (COVID-19) is an infectious disease caused by a newly discovered strain that mainly affects the upper respiratory system which is primarily spread through respiratory droplets. Patients affected with COVID that end up on mechanical ventilation may develop COVID Pneumonia which progresses to acute respiratory distress syndrome (ARDS). The lungs become inflamed and fill with fluid, making oxygen diffusion in capillaries difficult. For mechanically ventilated adults with COVID-19 and ARDS, lung protective strategies are recommended - low tidal volume (VT) ventilation (4–8 mL/kg of predicted body weight), plateau pressures of <30 cm H2O, conservative fluid strategy, higher positive end-expiratory pressure strategy, avoidance of routine use of inhaled nitric oxide, and ultimately prone ventilation in those refractory to treatment. Long term sequelae of COVID-19 are still unknown. When evaluating those with a history of ARDS or people who had SARS/Middle East Respiratory Syndrome, it may be deduced that those who suffer from COVID-19 may also have persisting lung abnormalities including, but not limited to substantial lung fibrosis.