2021 FSA Posters
P020: DESIGN AND DEVELOPMENT OF A MIXED REALITY SIMULATOR FOR REGIONAL ANESTHETIC BLOCKS OF THE HEAD AND NECK
Anthony J DeStephens, MSME; David Lizdas, BS; William Johnson, BS; Ilana Zarour, BS; Samsun Lampotang, PhD; Cameron Smith, PhD, MD; University of Florida
Introduction: The pterygopalatine ganglion (PPG), often described as the “Piccadilly Circus of the face” is of great importance to anesthesiologists, pain physicians, neurologists and surgeons, and its blockade is becoming more and more popular as our understanding of the mechanisms of headache improve. Recent publications have shed important light on its role in the pathophysiology of vascular or primary headaches. Pterygo-palatine ganglion block (PPGB) can be used for postoperative pain management for surgeries such as cleft palate, maxillary osteotomy, functional endoscopic sinus surgery and even tonsillectomy. To our knowledge, there is no commercially available simulator to practice such procedures. Therefore, we have developed a novel mixed reality simulator for teaching, as well as use as a potential research tool for exploring novel tools and techniques for regional anesthetic blocks of the head and neck.
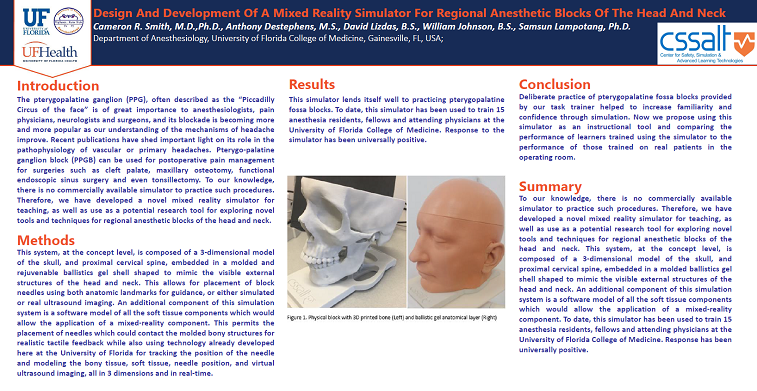
Methods: This system, at the concept level, is composed of a 3-dimensional model of the skull, and proximal cervical spine, embedded in a molded and rejuvenable ballistics gel shell shaped to mimic the visible external structures of the head and neck. This allows for placement of block needles using both anatomic landmarks for guidance, or either simulated or real ultrasound imaging. An additional component of this simulation system is a software model of all the soft tissue components which would allow the application of a mixed-reality component. This permits the placement of needles which could contact the molded bony structures for realistic tactile feedback while also using technology already developed here at the University of Florida for tracking the position of the needle and modeling the bony tissue, soft tissue, needle position, and virtual ultrasound imaging, all in 3 dimensions and in real-time.
Results: This simulator lends itself well to practicing pterygopalatine fossa blocks. To date, this simulator has been used to train 15 anesthesia residents, fellows and attending physicians at the University of Florida College of Medicine. Response to the simulator has been universally positive.
Discussion: Deliberate practice of pterygopalatine fossa blocks provided by our task trainer helped to increase familiarity and confidence through simulation. Now we propose using this simulator as an instructional tool and comparing the performance of learners trained using the simulator to the performance of those trained on real patients in the operating room.