2021 FSA Posters
P025: EFFICACY OF SEROTONIN-NOREPINEPHRINE REUPTAKE INHIBITORS (SNRIS) FOR MIGRAINE AND VESTIBULAR MIGRAINE PREVENTION
Jared Herman1; Emma Hall2; John Michael3; Omar Viswanath4; Alan Kaye5; Ivan Urits6; 1Mount Sinai Medical Center; 2Nova Southeastern University College of Osteopathic Medicine; 3Lake Erie College of Osteopathic Medicine - Bradenton; 4Valley Anesthesiology and Pain Consultants; 5Louisiana State University Health Shreveport, Department of Anesthesiology; 6Beth Israel Deaconess Medical Center, Department of Anesthesiology, Critical Care and Pain Medicine

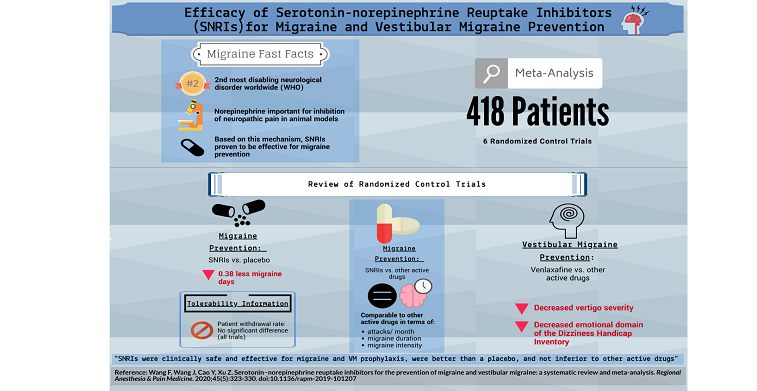
Introduction/ Background: This infographic summarizes a systematic review and meta-analysis of SNRIs in the prevention of migraine and vestibular migraine. Serotonin-norepinephrine reuptake inhibitors (SNRIs) are a widely used antidepressant that block the reuptake of serotonin and norepinephrine. Serotonin is known to play a role in migraine pathogenesis and Norepinephrine has been demonstrated to be an important inhibitor of neuropathic pain in animal models. Together, these mechanisms have led to the investigation of the role of SNRIs in migraine prophylaxis.
Methods: An updated review was performed focusing on the efficacy and tolerability of SNRIsfor migraine and vestibular migraine (VM) prevention. A search of PubMed, Web of Science and Cochrane Library databases was performed. Migraine frequency was the primary outcome while the Dizziness Handicap Inventory (DHI) scores and Vertigo Severity Scores (VSSs) were utilized for VM.
Results: Overall, six randomized controlled trials were analyzed. Of the 418 total patients analyzed, those receiving SNRIs had less migraine days (standardized mean difference -0.38). The effects of other SNRIs and other active drugs were comparable. For VM patients, venlaxafine demonstrated a significant advantage over other active drugs in decreasing VSS. The emotional domain score of the DHI was also decreased with venlaxafine. There was no significant difference in the rate of withdrawals due to side effects between SNRIs and other active drugs. There was also no significant difference in withdrawal rate due to side effects between SNRIs and a placebo
Discussion/ Conclusion: It can be concluded that SNRIs are clinically safe and display efficacy for migraine and VM prophylaxis. SNRIs were better than a placebo and not inferior to any other active drug. SNRIs may be a better choice for VM patients with coexisting psychiatric disorders.