2021 FSA Posters
P026: SPONTANEOUS PULMONARY EMBOLISM LEADING TO SUDDEN CARDIAC ARREST AND PERI-MORTEM C-SECTION IN A 39 WEEKS PARTURIENT DURING INDUCTION OF LABOR: A CASE REPORT
Onassis C Naim, MD; Cameron P Howard, MD; Maria Frosth, MD; Jeannie Miles, MD; B T Houseman, PhD, MD; Memorial Healthcare System
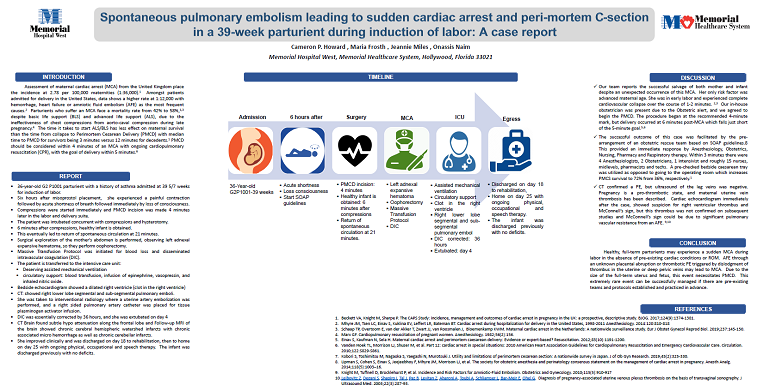
Introduction: Intra-partum Maternal Cardiac Arrest (MCA) is a rare event with an incidence of 0.8 per 100,000 deliveries (1). MCA is most commonly due to trauma, pulmonary embolus (PE), amniotic fluid embolus (AFE) or severe preeclampsia (2,3). Perimortem cesarean delivery (PMCD) is performed in up to 87% of cases of MCA, with significant morbidity and mortality for both mother and infant (4). Here we report the successful salvage of mother and infant following asystolic MCA and PMCD.
Case Report: A 36-year-old G2 P1001 was admitted at 39 5/7 weeks for induction of labor with misoprostol. Six hours following admission, she experienced a painful contraction followed by shortness of breath and immediate loss of consciousness. EKG showed asystole, OB ACLS was initiated, and an obstetric rescue alert was called. PMCD incision was made 4-minutes later in the labor suite, and the patient was intubated concurrent with compressions and hysterotomy. A viable infant was delivered 6-minutes following initiation of OB ACLS.
Following PMCD, the mother remained in asystole. ACLS was continued until ROSC was achieved at 21 minutes. She was transferred to the operating room due to persistent hypotension and bleeding, and massive transfusion protocol was initiated. Following evacuation of an adnexal hematoma, the patient was transferred intubated to the intensive care unit. Bedside echocardiogram showed a dilated right ventricle, McConnell's sign, and high suspicion for clot in the right ventricle. CT showed right lower lobe segmental and sub-segmental pulmonary emboli. Uterine artery embolization was performed, and a pulmonary artery catheter was placed for infusion of tPA.
The patient’s coagulopathy was corrected by 36 hours and she was extubated on postpartum day 4. MRI of brain showed chronic cerebral hemispheric watershed infarcts with chronic associated micro hemorrhage and chronic cerebellar infarcts. She was discharged on day 18 to rehabilitation, then home on day 25 with ongoing physical, occupational and speech therapy. The infant was discharged home with no deficits.
Discussion: Sudden MCA during in the absence of pre-existing cardiac conditions or rupture of membranes is extremely rare. In this case, unknown placental abruption could have resulted in AFE, or dislodgment of thrombus in uterine or deep pelvic veins may have led to PE. The cause remains unclear, as ultrasound of her leg veins was negative and right ventricular thrombus noted on bedside echocardiogram was not confirmed on subsequent studies.
This case illustrates how highly reliable systems facilitated a favorable outcome for both mother and infant following asystolic MCA, PMCD, prolonged ACLS, and DIC. Elements of this systems include practiced, multidisciplinary maternal response team (recommended by Society of Obstetric Anesthesia and Perinatology guidelines), pre-made surgical packs for rapid cesarean delivery, robust massive transfusion protocols, and the presence of an in hospital intensivist.
Mhyre JM, Tsen LC, et al. 2014:120:810-818
Schaap TP, Overtoom E, et al. Eur J Obstet Gynecol Reprod Biol. 2019; 237:145-150.
Einav S, et al. 2012;83(10):1191-1200.
Lipman S, Cohen S, et al. Anesth Analg. 2014;118(5):1003–16.