2021 FSA Posters
P027: MANAGEMENT OF URGENT PRE-TERM CESAREAN DELIVERY IN A PATURIENT WITH PRIOR LUNG RESECTION, SEVERE PROGRESSIVE PERIPARTUM CARDIOMYOPATHY AND PULMONARY HYPERTENSION
Taimoor A Khan, MD1; Rebecca Anderson, MD2; George Semien, MD, MPH, FASA2; Jean Miles, MD, FASA2; Xiwen Zheng2; Bejamin Houseman, MD, PhD, FASA2; 1Memorial Healthcare System; 2Envision Physician Services
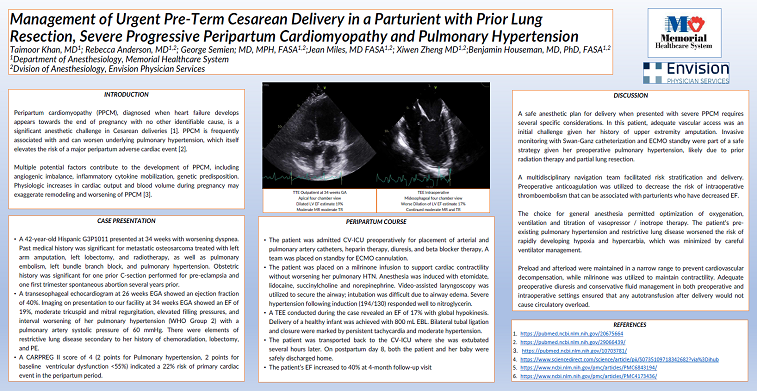
Introduction: This case report describes management of urgent, pre-term cesarean delivery in a patient with prior lung resection, peripartum cardiomyopathy (PPCM) and severe pulmonary hypertension (PAH). PPCM is diagnosed based on peripartum systolic heart failure without another identifiable cause and is frequently associated with worsening PAH [1,2]. This patient was referred to our service at 34 weeks gestation for multidisciplinary management due to worsening functional status in setting of prior lung lobectomy and reduced ejection fraction, and CARPREG II risk score of 5 (late assessment = 1, ventricular failure = 2, pulmonary hypertension = 2), which placed her at >40% risk for a primary peripartum cardiac event [3].
Case Report: A 42-year-old G3P1011 Hispanic female presented with an ejection fraction of 19% (decreased from 40% at 26 weeks gestation), moderate tricuspid and mitral regurgitation, and severe PAH (PASP 60 mmHg; WHO group 2). Past medical history was significant for prior pulmonary embolism, left bundle branch block, and metastatic osteosarcoma treated with left arm amputation, left lung lobectomy, and adjuvant chemotherapy. Past obstetric history was significant for prior c-section due to pre-eclampsia and one prior first trimester spontaneous abortion.
Our multidisciplinary team recommended urgent c-section under general anesthesia with ECMO available on standby. Prior to c-section, she was admitted to the cardiovascular ICU for optimization of anticoagulation / heart failure / pulmonary hypertension as well as placement of an arterial line and pulmonary artery catheter for hemodynamic monitoring. A milrinone infusion was initiated to support cardiac contractility without worsening PAH. Anesthesia was induced with etomidate, succinylcholine, and norepinephrine. Hypertension during laryngoscopy was treated with nitroglycerin. TEE imaging revealed an EF of 17% with global hypokinesis and permitted titration of fluid / inotrope / vasopressor therapy. A viable infant was delivered, and the patient was transferred to the ICU intubated for continued management of PPCM, PAH, anticoagulation, and pain. She was extubated several hours later, and both mother and infant were discharged home on postpartum day 8.
Discussion: This case report illustrates the importance of risk assessment and multidisciplinary planning in the urgent cesarean delivery of a parturient with prior lung resection, PAH, and severe PPCM. Invasive monitoring in both the OR and ICU permitted peripartum management of PPCM, PAH, and fluid shifts, while endotracheal anesthesia permitted TEE imaging and if needed, inhaled nitric oxide. Adequate diuresis and conservative fluid management ensured that autotransfusion after delivery did not cause circulatory overload in this patient with reduced lung volume.
Citations:
- https://pubmed.ncbi.nlm.nih.gov/20675664/
- https://pubmed.ncbi.nlm.nih.gov/29066439/
- https://pubmed.ncbi.nlm.nih.gov/29793631/