2021 FSA Posters
P028: ANESTHETIC MANAGEMENT OF A PARTURIENT WITH RECURRENT PULMONARY ARTERY SARCOMA AND SEVERE PULMONARY HYPERTENSION FOR CESAREAN SECTION: A CASE REPORT
Gianfranco Molfetto, DO1; George Semien, MD, MPH, FASA2; Michale Aguad, BS3; Jean Miles, MD, FASA2; Robert Brooker, MD2; Xiwen Zheng, MD2; 1Memorial Healthcare System; 2Envision Physician Services; 3Florida International University
Introduction: Pulmonary artery sarcoma (PAS) is an extremely rare tumor that is frequently asymptomatic until significant pulmonary artery obstruction and pulmonary hypertension occur (1). In parturients with PAS, symptoms worsen during late pregnancy, when total blood volume can increase up to 48% (2). This case report describes the risk stratification, multidisciplinary management and successful cesarean delivery of parturient with recurrent PAS.
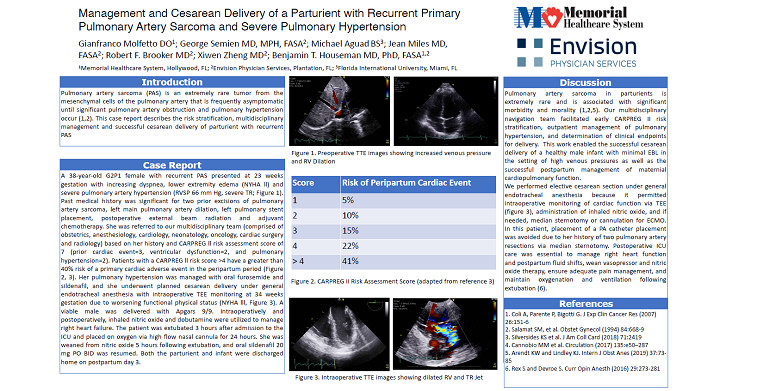
Case Report: A 38-year-old G2P1 female with recurrent PAS presented at 23 weeks gestation with increasing dyspnea, lower extremity edema (NYHA ll) and severe pulmonary artery hypertension (RVSP 66 mm Hg, severe TR). Past medical history was significant for two prior excisions of pulmonary artery sarcoma, left main pulmonary artery dilation, left pulmonary stent placement, postoperative external beam radiation and adjuvant chemotherapy. She was referred to our multidisciplinary team (comprised of obstetrics, anesthesiology, cardiology, neonatology, oncology, cardiac surgery and radiology) based on her history and CARPREG ll risk assessment score of 7 (prior cardiac event=3, ventricular dysfunction=2, and pulmonary hypertension=2). Patients with a CARPREG ll risk score > 4 have a greater than 40% risk of a primary cardiac adverse event in the peripartum period (3). Her pulmonary hypertension was managed with oral furosemide and sildenafil, and she underwent planned cesarean delivery under general endotracheal anesthesia at 34 weeks gestation due to worsening functional physical status (NYHA lll). A viable male was delivered with Apgars 9/9. Intraoperatively and postoperatively, inhaled nitric oxide and dobutamine were utilized to manage right heart failure (fig 1). The patient was extubated 3 hours after admission to the ICU and placed on oxygen via high flow nasal cannula for 24 hours. She was weaned from nitric oxide 5 hours following extubation, and oral sildenafil 20 mg PO BID was resumed. Both the parturient and infant were discharged home on postpartum day 3. Postoperative cardiology followup was scheduled in 4 weeks.
Discussion: Pulmonary artery sarcoma in parturients is extremely rare and is associated with significant morbidity and morality (1,2). Our multidisciplinary navigation team facilitated early risk stratification, management of pulmonary hypertension, determination of clinical endpoints for delivery, and formulation of successful delivery and postoperative care plans (4,5). We performed elective cesarean section under general endotracheal anesthesia because it permitted intraoperative monitoring of cardiac function TEE, administration of inhaled nitric oxide, and if needed, median sternotomy or cannulation for ECMO. In this patient, placement of a PA catheter placement was avoided due to her surgical history. Postoperative ICU care was essential to manage right heart function and postpartum fluid shifts, wean vasopressor and nitric oxide therapy, ensure adequate pain management, and maintain oxygenation and ventilation following extubation (6).
1. Coli A, Parente P, Bigotti G. J Exp Clin Cancer Res (2007) 26:151-6
2. Salamat SM, et al. Obstet Gynecol (1994) 84:668-9
3. Silversides KS et al. J Am Coll Card (2018) 71:2419
4. Cannobio MM et al. Circulation (2017) 135:e50–287
5. Arendt KW and Lindley KJ. Intern J Obst Anes (2019) 37:73-85
6. Rex S and Devroe S. Curr Opin Anesth (2016) 29:273-281