2021 FSA Posters
P030: QUALITY IMPROVEMENT: DECREASING ASA PHYSICAL STATUS CLASSIFICATION ELECTRONIC MEDICAL RECORD DOCUMENTATION ERROR
Jose A Alfonso, BSc; Ferenc Rabai, MD; Michael Caouette, MS; Stephanie Gore, MSN, CCRN, RN; Katherine Cairnes, MHA; Nikolaus Gravenstein, MD; University of Florida College of Medicine
Introduction/Background: In 2010, there were 51.4 million surgical procedures performed in the United States in the inpatient setting. Accurate documentation of surgery type is required for precise medical coding/billing and calculation of hospital case mix index. The American Society of Anesthesiologist Physical Status (ASA PS) classification system defines emergency surgery as existing when delay in treatment of the patient would lead to a significant increase in threat to life or body part. In this quality improvement study, we aim to improve electronic medical record (EMR) workflow and reduce documentation error of emergency surgery by anesthesiology providers. We hypothesize that by simplifying ASA PS classification EMR data entry, we will thereby lower cognitive load on the provider resulting in lower documentation error of emergency surgery.
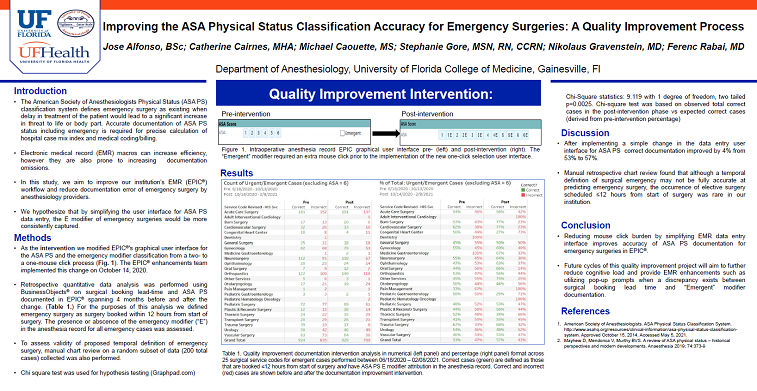
Methods: Modified EMR graphical user interface from a two- to a one-mouse click process, where ASA PS classification and emergency modifier could be selected simultaneously in the pre- and intra-operative record. Defined emergency surgery as surgery scheduled ≤12 hours from start of surgery. Performed retrospective pre- and post-intervention data analysis examining changes in counts of correct and incorrect emergency surgery attribution in the anesthesia record. Performed qualitative retrospective manual chart review on random subset of data (200 total cases) collected to assess limitations of proposed temporal definition of emergency surgery.
Results: Retrospective quantitative analysis of preliminary data was obtained across 25 categories of surgical services, with a total of 3,397 emergency surgical cases identified starting from June 18th, 2020 to February 8th, 2021, or approximately four calendar months before and after intervention. Pre-intervention data collected from June 18th, 2020 to October 13th, 2020 showed cumulative 53% correct response. Post-intervention data, including start day of intervention, from October 14th, 2020 to February 8th, 2021 showed cumulative 57% correct response.
Discussion/Conclusion: Retrospective pre- and post-interventional preliminary results showed improvement in correct documentation of emergency surgery. Manual retrospective chart review showed that although a temporal definition of surgical emergency may not be fully accurate at predicting emergency surgery, the occurrence of elective surgery scheduled ≤12 hours from start of surgery is minor in comparison.