2021 FSA Posters
P031: HOW PPE TYPE AND HEALTHCARE WORKER CHARACTERISTICS IMPACT PERIOPERATIVE COMMUNICATION
Onassis Naim, MD1; Benjamin Houseman, MD1; Michael Aguad, BS2; Cameron Howard, MD, CPE, FASA3; Walter Diaz3; Xiwen Zheng3; Maria Frosth, MD3; 1Memorial Healthcare System; 2Florida International University; 3Envision Physician Services
INTRODUCTION: The use of extensive PPE for the care of patients with SARS-CoV-2 has impaired the ability of healthcare workers to communicate effectively, representing a risk to patient safety (1-4). It is unclear whether types of PPE or characteristics of healthcare providers impact the ability to communicate. This abstract examines how types of PPE and healthcare worker characteristics impact communication, as well as the ability of an Iasus GP-3 throat microphone to improve communication in the perioperative setting.
METHODS: 75 staff members at Memorial Hospital West completed a 19-item survey to assess the impact of gender, age, healthcare role (preop / OR / recovery nursing, surgeon, surgery assistant, anesthesia), native language (English, other), respirator type (N95, P100) and eye protection type (face shield, goggles) on perception of communication. The Bamford-Kowal-Bench (BKB) sentence list, a benchmarked tool for evaluating comprehension of verbal communication, was utilized to quantitatively analyze communication between male and female healthcare workers (41-50 year old; male native and non-native English speaker, female native and non-native English speaker). Variables included distance between workers (3 versus 6 feet), phone versus in person communication, and ambient noise level (60 dB, 90dB). An Iasus GP3-R throat microphone was utilized for speakers to assess its efficacy as an intervention. Data were analyzed using Microsoft Power BI.
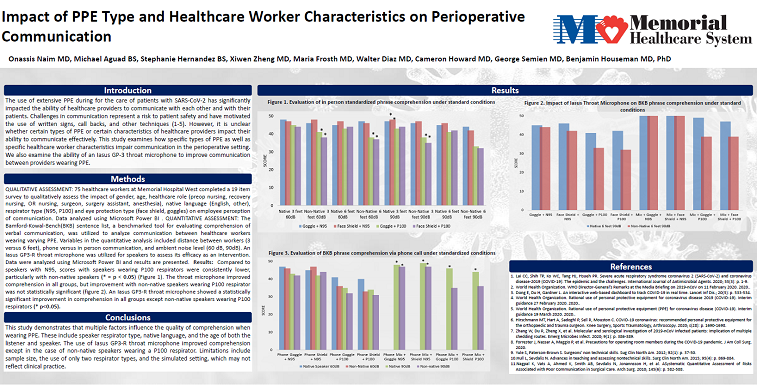
RESULTS: Survey responses were not statistically different between male and female workers, nor were they statistically different between native English speakers and non-native English speakers. However, results were statistically different (p=0.04) between younger cohorts (21-30, 31-40 year-old) and more mature workers (41-50, 51-60 year-old). These differences appeared in both speaker and listener roles. In this survey there was a non-statistically significant difference between individuals who routinely wore P100 respirators and those who wore N95 (p=0.12).
Comprehension of BKB phrases was impacted primarily by native speaker status and type of respirator under conditions tested. Non-native speakers wearing P100 respirators were more poorly understood under most conditions. Gender of speaker did not influence these results.
An Iasus GP-3 throat microphone was utilized to improve in person BKB phrase comprehension (6 feet, 90 dB). The throat microphone produced a statistically significant improvement in comprehension of all speakers, but failed to improve the comprehension of non-native speakers wearing P100 respirators. During phone conversation, the throat microphone again produced a statistically significant improvement in comprehension in all groups except non-native speakers wearing P100 respirators.
CONCLUSION: This study demonstrates that multiple factors influence the quality of comprehension when wearing PPE. These include respirator type and native language of speaker, and the age of both the listener and speaker. The use of Iasus GP3-R throat microphone improved comprehension except in the case of non-native speakers wearing a P100 respirator. Limitations include sample size, the use of only two respirator types, use of non-native Spanish speakers, and the simulated setting.
1. World Health Organization. Interim guidance 19 March 2020. 2020.
2. Arthroscopy. 2020; s(28): p. 1690-1698.
3. J Am Coll Surg. 2020 Jun;230(6):1098-1101
4. Surg Clin North Am. 2015; 95(4): p. 869-884.