2021 FSA Posters
P032: EFFICACY OF EPINEPHRINE TEST DOSE IN THE PREVENTION OF LOCAL ANESTHETIC SYSTEMIC TOXICITY
Sandy Ren, MD1; Ralf E Gebhard, MD, FASA2; 1Jackson Memorial Hospital & University of Miami; 2University of Miami
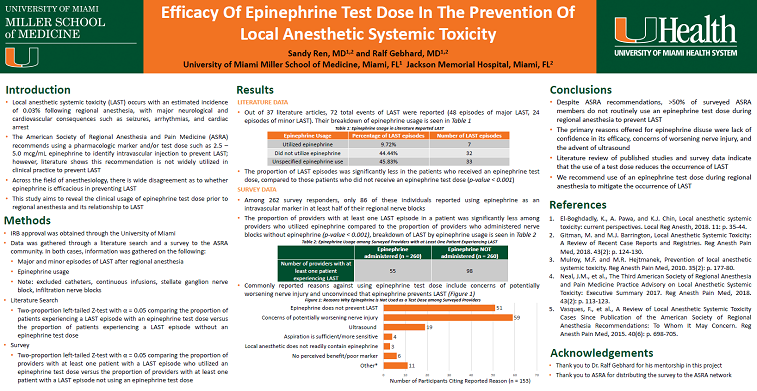
Introduction/Background: LAST has an estimated incidence of 0.03% following the use of regional anesthesia, with major consequences in neurological and cardiovascular systems such as seizures, arrhythmias, or cardiac arrest. The American Society of Regional Anesthesia and Pain Medicine (ASRA) recommends using an epinephrine test dose as a marker to identify accidental intravascular injection of peripheral anesthesia to prevent LAST and reduce mortality. We believe this test dose is not widely used in practice due to controversy about its ability to prevent LAST.
Methods: Literature dating back to the year 2000 was reviewed and a survey of the ASRA community (IRB approval and consents were obtained) was performed. Descriptive statistics was used to summarize the data and two proportion Z-tests (α = 0.05) were utilized to assess whether there was (1) a statistically significant difference in the proportion of patients experiencing LAST episodes when receiving an epinephrine test dose compared to those without an epinephrine test dose in literature and (2) a statistically significant difference in the presence of LAST episodes among the proportion of providers who utilized epinephrine compared to those who did not use epinephrine in survey data.
Results: Among cases of reported LAST between 2000-2019, 44.44% of patients did not receive an epinephrine test dose, 9.72% received an epinephrine test dose, and 45.83% case authors could not be reached for clarification regarding epinephrine usage. A two-proportion Z-test revealed a significantly smaller proportion of patients experiencing LAST when given an epinephrine test dose, compared to patients experiencing LAST who did not receive an epinephrine test dose (p < 0.001). Among those surveyed in the ASRA community, 54.96% of providers reported never having used an epinephrine test dose during regional anesthesia. Of the 121 providers who reported LAST, there were 545 minor episodes of LAST (such as mental status change, perioral numbness/tingling, ringing in the ears, and metallic taste) and 92 major episodes of LAST (seizure and cardiac complications). Two-proportion Z-test indicated a statistically significant smaller proportion of providers reporting LAST episodes among those who administered nerve blocks with epinephrine compared to those who did not utilize an epinephrine test dose (p < 0.001).
Discussion/Conclusion: Despite ASRA’s formal recommendation to use an intravascular marker such as epinephrine when administering regional anesthesia to prevent LAST, our study shows that >50% of users do not routinely utilize the test dose due to commonly cited reasons such as lack of confidence in its efficacy, concerns of worsening nerve injury, the advent of ultrasound, among others. Both our literature search and survey data affirm the importance of ASRA’s recommendation to use an intravascular marker such as epinephrine to prevent LAST, as indicated by its statistically significant success in reducing both the proportion of patients experiencing LAST and proportion of providers with LAST episodes. It is our recommendation to utilize an epinephrine test dose during the administration of regional anesthesia to prevent potentially lethal episodes of LAST.