2021 FSA Posters
P033: PERIOPERATIVE SEIZURE
Katherine M Medrano, MD; Joohi Khan, MD; Nicholas Nedeff, MD; Kendall Regional Medical Center
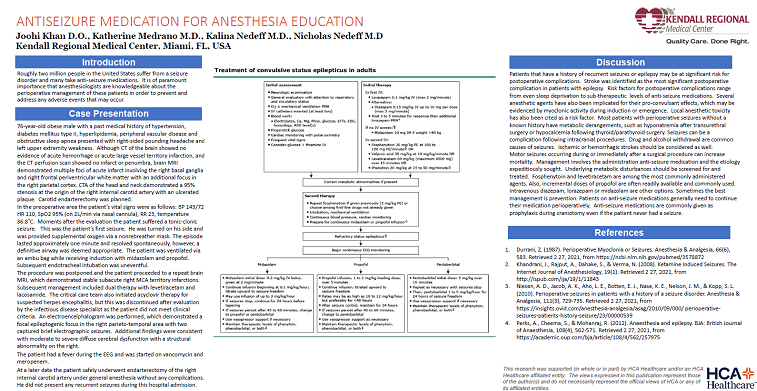
Introduction: Many individuals in the United States have history of seizure disorder, many are on antiseizure medication for symptom management. It is paramount that anesthesiologists are aware of these disorders and understand the mechanism of these disorders as well as how to prevent or manage any adverse perioperative events that may occur.
Methods: 76 yo M with PMH hypertension, DM II, hyperlipidemia, peripheral vascular disease, OSA presented to the preoperative area for right carotid endarterectomy. The patient originally presented to the hospital complaining of right sided pounding headache accompanied with left upper extremity weakness, presenting as a stroke alert however on CT of brain there was no evidence of acute hemorrhage or acute core infarct, CTA Head and Neck demonstrated a 95% stenosis at the origin of the right internal carotid artery. Patient was made NPO the night before his surgery and presented to the preoperative holding area the morning of the procedure. Patient vitals were BP 143/72 HR 110 Pulse Ox 95% on 2L/min via NC RR 23 Temperature 36.8. After evaluation, patient was seen by nursing staff having tonic clonic movements.
Results: The patient was positioned laterally and provided supplemental oxygen by nonrebreather mask. The episode lasted approximately one minute, and the seizure ceased without treatment. Patient was requiring assistance with ventilation via ambu bag, the patient was given midazolam and propofol, the decision was made to proceed with endotracheal intubation. Intubation was uneventful. Careful maintenance of vital signs including blood pressure was cautiously preserved. Surgery was cancelled, as this was the patient’s first seizure, the patient was taken for imaging and further studies.
Discussion: Patients with history of seizures are at significant risk for postoperative complications. Stroke was identified as the most significant postoperative complication in patients with epilepsy. There are multiple reasons that a seizure may occur during the perioperative period, the most prominent risk factor being poor seizure control prior to surgery. If the patient is on antiseizure medication and they have subtherapeutic drug levels, or even sleep deprivation they can be at increased risk for seizure. Several anesthetic agents have been implicated for their proconvulsant effects, which may be evidenced by myoclonic activity during induction or emergence. Local anesthetic toxicity is also an implication. Most patients with perioperative seizures without known history have metabolic derangements, like hyponatremia after transurethral surgery, hypocalcemia following thyroidectomy /parathyroidectomy. Seizures can be a complication following intracranial procedures. Drug and alcohol withdrawal are common causes of seizures. Ischemic or hemorrhagic strokes should be considered as well. Seizures should be managed, as seizures occurring during or immediately after a surgical procedure can increase mortality. Antiseizure medication is quickly administered and the cause for the seizure should be determined. Underlying metabolic disturbances should be checked and treated. Fosphenytoin, and levetiracetam, are commonly administered, propofol in small incremental doses is readily available. Intravenous diazepam, lorazepam/midazolam are other options. Best management is prevention. Antiseizure medications must be continued perioperatively. Antiseizure medications are given as prophylaxis during craniotomy even if never had a seizure.