2021 FSA Posters
P035: CONTINUOUS STELLATE GANGLION BLOCKADE TO THE RESCUE
Ankit Bhatia, DO1,2; Pranav Deshpande, MD1; Maria Suarez, MD1; Ralf Gebhard1; 1Universty of Miami; 2Jackson Memorial Hospital
Intro: The stellate ganglion is a sympathetic ganglion formed from the fusion of the inferior cervical and superior thoracic ganglia, providing most of the sympathetic innervation to the upper extremity including the head and neck. Blockade of the stellate ganglion is often used to diagnosis and manage various sympathetically mediated pain states such as CRPS and phantom limb pain, however, may also be used for refractory angina and prevention of vasospasm.
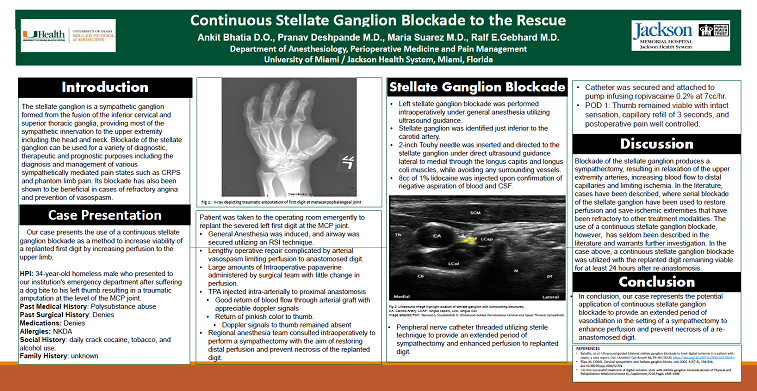
Case Presentation: Our case presents the use of a continuous stellate ganglion block as a method to increase perfusion to the upper limb to increase the viability of a replanted thumb. Our patient is a 34-year-old homeless male with a medical history significant for polysubstance abuse including daily crack cocaine, tobacco, and marijuana use who presented to our institutions emergency department after sustaining a dog bite to his left thumb resulting in a traumatic amputation at the level of the MCP joint. The severed thumb was found 10 minutes after the incident by a bystander and placed directly on ice. Patient was subsequently taken to the operating room emergently in an attempt for replantation of the severed left thumb at the MP joint. The lengthy operative repair was complicated by arterial vasospasm limiting perfusion to the anastomosed thumb despite the administration of large amounts of intraoperative papaverine. Surgical team subsequently injected TPA intra-arterially to the proximal anastomosis which resulted in good return of blood flow through the arterial graft with appreciable doppler signals. Doppler signals to the thumb remained absent, however a return of pinkish color was noted. Regional anesthesia team was subsequently consulted intraoperatively to perform a sympathectomy to prevent further vasospasm. A left stellate ganglion block was performed intraoperatively under general anesthesia, using ultrasound guidance. The stellate ganglion was identified just inferior to the carotid artery. A 2-inch Tuohy needle was inserted in-plane under direct ultrasound guidance lateral to medial through the longus capitis and longus coli muscles carefully to prevent injury to surrounding vessels. Upon confirmation of negative aspiration for blood or CSF, 8cc of 1% lidocaine was injected. A peripheral nerve catheter was subsequently placed using sterile technique to prevent vasospasm postoperatively and improve flow to the replanted digit to increase chance of viability. Catheter was secured and attached to a pump running ropivacaine 0.2% with a rate of 7cc/hr, and patient was subsequently extubated and transferred to the ICU on replant protocol. On postoperative day 1, thumb remained viable with intact sensation, a capillary refill of 3 seconds, and postoperative pain adequately controlled.
Conclusion: In conclusion, our case represents the potential use of a stellate ganglion catheter to allow for an extended period of vasodilation in the setting of a sympathectomy to enhance perfusion and increase viability of a replanted digit.