2021 FSA Posters
P037: AN ATYPICAL PRESENTATION OF INCOMPLETE SPINAL ANESTHESIA
Michael Leclerc, DO; Ali Ahmed-Elamin; Tianyu Jiang, DO; Oak Hill Hospital
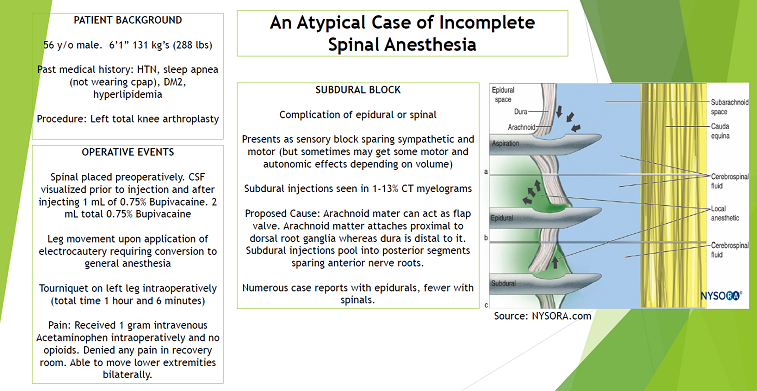
Patient is a 56-year-old male with history of hypertension, diabetes mellitus 2, obstructive sleep apnea (non-compliant with CPAP), and hyperlipidemia who underwent left total knee arthroplasty with spinal anesthesia as the mode of anesthesia. During spinal anesthesia adequate cerebrospinal flow was observed and patient was administered 2 mL of 0.75% bupivacaine. Following spinal anesthesia patient laid supine and put to sleep with propofol infusion. Surgery started and upon application of electrocautery the patient’s leg moved. Concern for failed spinal arose and the case was converted to general anesthesia. Perioperatively the patient received 1 gram of intravenous acetaminophen for pain and despite possibility of failed spinal anesthesia denied any pain postoperatively. Blood pressure dropped mildly following initiation of general anesthesia, however this drop resolved following cessation of volatile anesthetics. Likewise, postoperatively patient had no apparent loss of strength in lower extremities bilaterally. Given the findings it is possible that the injected local anesthetic went subdural as opposed to intrathecal.
This case is unique in that it demonstrates the possibility of a subdural block, infiltration of local anesthetic into the subdural space instead of the epidural or intrathecal spaces. Most case reports regarding subdural blocks are with epidurals however few case reports do exist with it in regards to spinal anesthesia. The classic presentation is a pure sensory block occurring 15 to 20 minutes post-injection which extends cephalad but spares motor and autonomic fibers. The presentation is variable and can include variable effects on motor and autonomic fibers. When performing spinal anesthesia this can occur as a result of the dura mater functioning as a flap valve with injection. The supposed mechanism behind the presentation is related to the location of the attachment of the dura mater relative to the dorsal root ganglion in comparison to the arachnoid mater’s attachment. The dura mater attaches distal to the dorsal root ganglion whereas the arachnoid mater’s attachment is proximal. Therefore, any local anesthetic into this space will spread dorsally and bathe the posterior portion of nerve roots leading to a predominantly sensory block.
While most presentations involve extensive cephalad spread of local anesthetic, as mentioned previously most case reports are during placement of epidurals which involve higher volumes of local anesthetics than spinals, thus leading to extensive cephalad spread. Given the lack of motor block and autonomic effect in this patient, as well as no pain postoperatively despite zero narcotic use, it is plausible that this patient’s neuraxial injection resulted in a subdural block.