2023 FSA Podium and Poster Abstracts
P059: PULMONARY ARTERY CATHETER ENTRAPMENT DURING AN LVAD CASE
Mariana Rubini Silva Ceschim, MD; Oscar Aljure, MD; Mathias Bruefach, MD; Harish Ram, MD; University of Miami/Jackson Health System
Introduction: Pulmonary Artery Catheter (PAC) is used to guide therapy in critically ill patients. Despite many minimally invasive hemodynamic monitoring methods, as well as a lack of evidence supporting improved outcomes, PAC continues to be used in cardiac surgery and is a gold standard for measuring pulmonary artery pressures and cardiac output. Complications associated with its use are rare, however can be fatal. We report a case of an entrapped PAC.
Case Report: A 69-year-old male with ischemic cardiomyopathy presented for evaluation by the heart failure team. Two months prior he had a myocardial infarction and drug-eluting stent placement complicated by stent thrombosis and cardiogenic shock. Cardiothoracic surgery and heart failure teams determined he would benefit from left ventricular assist device placement.
The patient was taken to the operating room (OR) and underwent general anesthesia with continuous blood pressure monitoring. A right internal jugular vein 9 French introducer and a thermodilution PAC were placed uneventfully. After chest closure the patient became hypotensive with increased chest tube output. The surgeon decided to reopen the chest to achieve further hemostasis. At this time the CO was non-computational, and we noticed blood at the CO connector port (Figure 1).

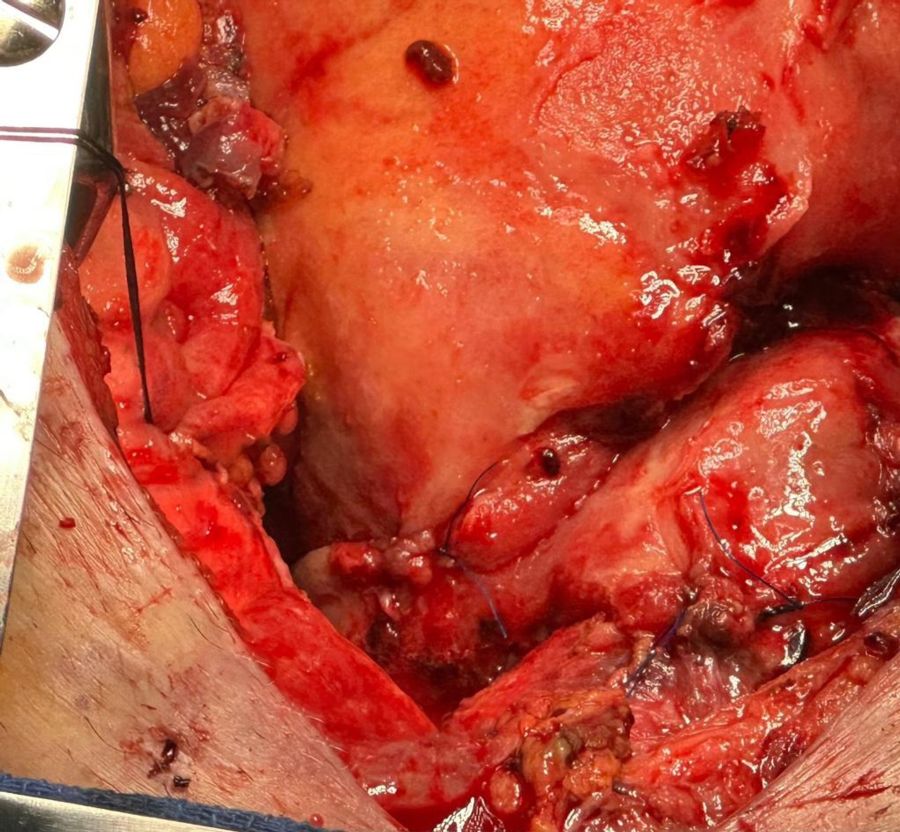
Patient regained hemodynamic stability and was taken to the intensive care unit (ICU). On the following day he was taken to the OR for washout, CO monitoring was still not computational, and PAC repositioning was not possible. The surgical team then noted that the PAC was inadvertently sutured to the heart (Figure 2). After suture removal, PAC was removed successfully.
Discussion: Complications related to PAC use occur in approximately 0.03% to 1% of patients, and include coiling/knotting of the catheter, entrapment, pneumothorax, arrhythmias, carotid or pulmonary artery injury, and infection. One uncommon complication is PAC entrapment with an incidence of approximately 0.065%. Surgical removal is almost always required and can be associated with significant morbidity and mortality, given these patients’ higher risk of infection and prolonged hospitalization.
Intraoperative indication of an entrapped PAC may include:
- inaccurate values on the PAC monitor noted after PAC manipulation in the surgical field (CO, SvO2 or temperature for instance), or
- blood noted in the non-communicating channel of PAC (thermistor connector, balloon inflation port, or optical module that connects to the fiberoptic SvO2 depending on which lumen is damaged by the entrapped suture)
Figure 1 indicates a clue to a breach in the thermistor lumen as evidenced by blood in the corresponding connecting port, with resultant inaccurate CO computation. This was most likely due to damage to PAC because of suture placement at the time of achieving hemostasis (Figure 3).
If entrapment is suspected when encountering resistance or hemodynamic instability during attempted removal, any sustained traction should be avoided as this could lead to hypotension, arrhythmia, perforation, and bleeding. Strategies to avoid this complication include frequent communication with the surgical team, routine retraction of the PAC and ensuring PAC mobility prior to chest closure.

