2023 FSA Podium and Poster Abstracts
P068: INTRAOPERATIVE MANAGEMENT OF CHANGING MOTOR-EVOKED POTENTIAL DURING SPINAL SURGERY AND MITIGATING POST OPERATIVE CONSEQUENCES: A CASE PRESENTATION
Christopher P Emerson, MD; Michael E Mahla, MD; UHealth, Department of Anesthesiology and Perioperative Pain Medicine
Introduction/Background: Intraoperative neurological monitoring (IONM) with somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) are commonly used during major spine surgery to monitor spinal cord function during manipulation of the spinal column. Studies have reported that intraoperative changes in SSEPs have been noted to occur in 2.5-6.5% of patients who undergo spinal column surgery. One large study found that 3.4% of patients who underwent corrective spinal deformity surgery had an IOMN alert, and 1.5% of patient’s showed significant suppression of MEP amplitude without changes to SSEP potentials compared to baseline, supporting the added benefit of MEP monitoring along with SSEP monitoring.
Methods: IOMN checklists have been validated to improve coordinated responses among anesthesiologists, surgeons, and neuromonitoring personnel when an IOMN alert is detected and all potential reversible causes corrected. We present a case of a 63-year-old man, ASA 3, BMI 33.9, who was scheduled to undergo elective laminectomy, bilateral foraminotomies, and fusion of Lumbar 4 to Sacral 1 with instrumentation for treatment of symptomatic compression of the neural foramina and nerve roots at L4/5 and L5/S1 refractory to conservative management. Intraoperatively, an IONM alert was triggered due to changes in lower extremity MEPs from baseline without any changes to SSEP signals.
Results: Total intravenous anesthesia (TIVA) was allowed to reach steady state before capturing the patient’s baseline SSEP and MEP signals in all extremities (Figure 1). Approximately 90 minutes after incision, MEP testing showed normal responses from the upper extremities and absent responses on the left lower extremity (LLE) with only a weak, relatively non-reproducible response in one muscle group on the right lower extremity (RLE) (Figure 2). After notifying both the surgeon and the anesthesiologist, the mean arterial pressure was increased by 20% utilizing phenylephrine infusion, with significant improvement in RLE MEPs (Figure 3). At the surgeon’s request, the patient was given three grams of methylprednisolone to reduce the potential for spinal cord swelling. For the following three hours the patients MEP and SSEP signals remained stable. As anesthesia was lightened as part of emergence, LLE MEP showed improvement (Figure 4). The patient was then awakened for extubation. Initially, he could not move his LLE, but rapidly improved in motor strength. He appeared neurologically intact in all extremities prior to leaving the operating room. The patient was then transferred to the post operative care unit for full recovery after anesthesia.
Discussion/Conclusion: A consensus statement from the American Society of Neurophysiologic Monitoring concluded that MEP monitoring in combination with SSEP monitoring is well established to prevent injury to sensory and motor tracts during spinal column surgery. Prompt identification and treatment of reversible causes of IOMN signals are paramount for minimizing the risk of persistent neurologic deficits relative to baseline. Successful postoperative outcome in our patient was achieved due to (1) utilization of multimodal IOMN, (2) detection of IOMN Alert, and (3) multidisciplinary strategy to treat reversible causes of the IOMN alert.
Figure 1
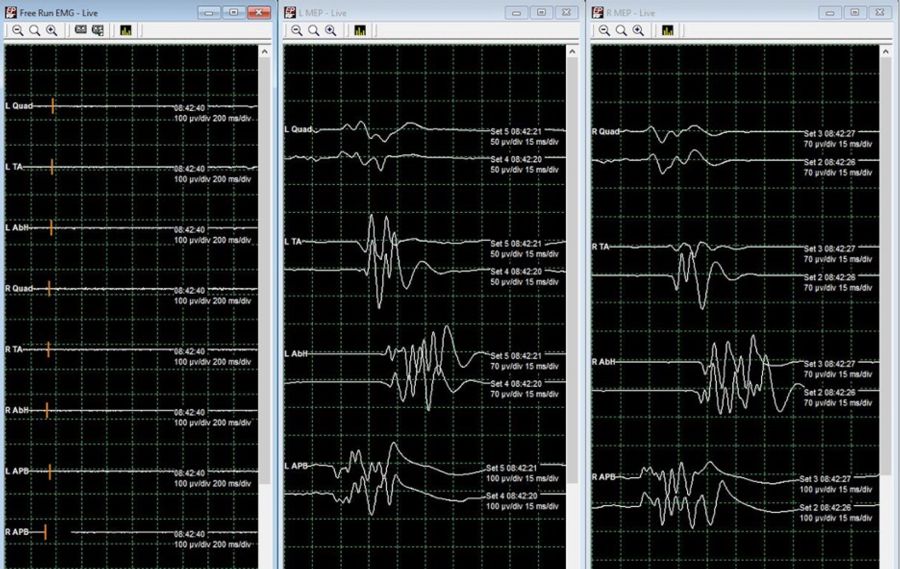
Figure 2

Figure 3

Figure 4

