2021 FSA Posters
P008: A CHALLENGING CASE OF ANAPHYLAXIS IN THE POST ANESTHESIA CARE UNIT
J Knapp, MD; A Vera Arroyo, MD; E Varga, MD; Jackson Memorial Hospital
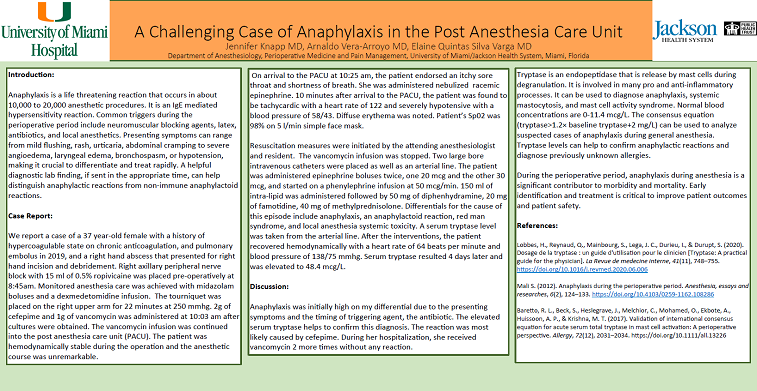
Introduction: Anaphylaxis is a life threatening reaction that occurs in about 10,000 to 20,000 anesthetic procedures. It is an IgE mediated hypersensitivity reaction. Common triggers during the perioperative period include neuromuscular blocking agents, latex, antibiotics, and local anesthetics. Presenting symptoms can range from mild flushing, rash, urticaria, abdominal cramping to severe angioedema, laryngeal edema, bronchospasm, or hypotension, making it crucial to differentiate and treat rapidly. A helpful diagnostic lab finding, if sent in the appropriate time, can help distinguish anaphylactic reactions from non-immune anaphylactoid reactions.
Case Report: We report a case of a 37 year-old female with a history of hypercoagulable state on chronic anticoagulation, pulmonary embolus in 2019, and a right hand abscess that presented for right hand incision and debridement. Right axillary peripheral nerve block with 15 ml of 0.5% ropivicaine was placed pre-operatively at 8:45am. Monitored anesthesia care was achieved with midazolam boluses and a dexmedetomidine infusion. The tourniquet was placed on the right upper arm for 22 minutes at 250 mmhg. 2g of cefepime and 1g of vancomycin was administered at 10:03 am after cultures were obtained. The vancomycin infusion was continued into the post anesthesia care unit (PACU). The patient was hemodynamically stable during the operation.
On arrival to the PACU at 10:25 am, the patient endorsed an itchy sore throat and shortness of breath. She was administered nebulized racemic epinephrine. 10 minutes after arrival to the PACU, the patient was found to be tachycardic with a heart rate of 122 and severely hypotensive with a blood pressure of 58/43. Diffuse erythema was noted. Patient’s Sp02 was 98% on 8 l/min simple face mask.
Resuscitation measures were initiated by the attending anesthesiologist and resident. The vancomycin infusion was stopped. Two large bore intravenous catheters were placed as well as an arterial line. The patient was administered epinephrine boluses twice, one 20 mcg and the other 30 mcg, and started on a phenylephrine infusion at 50 mcg/min. 150 ml of intra-lipid was administered followed by 50 mg of diphenhydramine, 20 mg of famotidine, 40 mg of methylprednisolone. Differentials for the cause of this episode include anaphylaxis, an anaphylactoid reaction, red man syndrome, and local anesthesia systemic toxicity. A serum tryptase level was taken from the arterial line. After the interventions, the patient recovered hemodynamically with a heart rate of 64 beats per minute and blood pressure of 138/75 mmhg. Serum tryptase resulted 4 days later and was elevated to 48.4 mcg/L.
Discussion: Anaphylaxis was initially high on my differential due to the presenting symptoms and the timing of triggering agent, the antibiotic. The elevated serum tryptase confirms this diagnosis. The inciting agent was most likely cefepime. During her hospitalization, she received vancomycin 2 additional times without any reaction. During the perioperative period, anaphylaxis during anesthesia is a significant contributor to morbidity and mortality. Early identification and treatment is critical to improve patient outcomes and patient safety.